It is very natural to daydream sometimes now or again; in fact, it happens to most individuals. However, for some who suffer from a mental illness known as “dissociation,” the reasons for their seeming detachment from reality are often much more nuanced.
When your mind becomes dissociated, it stops processing information normally. Disconnection from yourself, your emotions, your past, and your environment is a real possibility. Both your sense of self and the way you see time may be impacted.
Most of the time, the signs and symptoms disappear with time. Days, weeks, or even hours might pass. However, if you find that your dissociation is triggered by a traumatic event or a mental illness such as schizophrenia, it may be necessary to seek professional help.
What Are Symptoms of Dissociation?
Some people have amnesia or blank spots in their memories when dissociation is present. You can start to doubt your own reality or the reality of the physical world.
Alterations to your emotional state could also manifest as:
- Enjoy a transcendental experience
- On sometimes, you may feel as if someone else entirely
- Feel dizzy or as if your heart is racing
- Experience emotional detachment or numbness
- Have little to no discomfort
Other possible signs include:
- Feel time differently
- Forget the path you took to get there
- Keep your focus narrow
- Feel the presence of inner voices
- Experience vivid, lifelike flashbacks
- Stop moving
- Lose yourself in a fantastical universe that seems genuine
Causes of Dissociation
Trauma
If anything very terrible were to happen to you, you may mentally separate from the here and now. Peritraumatic dissociation describes this. This is a defense mechanism your mind employs to shield you from the traumatic event’s full effect, according to experts.
Some of the factors that might trigger peritraumatic dissociation include:
- Acts of sexual or bodily violence
- Abuse in childhood
- Combat
- Arrest or shackling
- Road traffic incidents
- Events caused by Mother Nature
Experiencing traumatic events repeatedly may lead to dissociative disorders, which are characterized by extreme dissociation. You could lose touch with reality, get temporarily disoriented, or even assume a new identity entirely in your head.
Hypnosis
If you ever find yourself lost in thought, you may be experiencing a kind of “auto-hypnotic state.” You could find that your physical awareness has diminished. You might enter a more profound dissociative state with other forms of hypnosis. For pain, anxiety, addictive habits, or post-traumatic stress disorder (PTSD), a qualified expert may recommend therapeutic hypnosis.
Certain drugs
Drunkenness and drug use may cause you to lose touch with reality and your sense of self. Psychedelic users, according to studies, can experience a transient dissociation from reality when they consume substances like LSD and psilocybin.
Meditation
Meditation, like daydreaming, may cause you to lose track of time and place. According to some seasoned meditators, there are mindfulness meditation techniques that cause them to forget about themselves and their bodies.
Related Mental Health Conditions
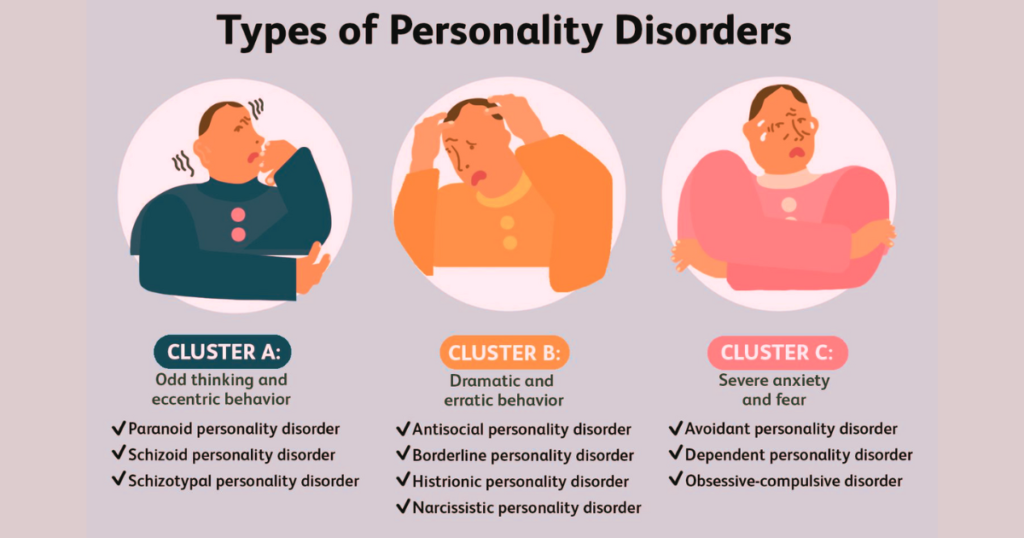
Dissociation from certain mental health conditions may be present in you. In addition to PTSD and schizophrenia, dissociation is associated with:
- Acute stress disorder
- Borderline personality disorder
- Affective disorders
- Obsessive-compulsive disorder
- Depression
- Eating disorders
Warning Signs
It is possible to experience dissociation without realizing it. For example, if you suffer from dissociative disorder, you could conceal or rationalize your symptoms.
Some common warning indicators that you or someone you care about should be aware of are:
- Extreme shifts in our mood
- Problems retaining certain information
- Neglecting to remember previous actions or words
- Modified identities are characterized by changes in behavior or ability.
- Anxiety, depression, or even a panic attack
- Suicidal or self-harming thoughts
- Drug misuse
- Ineffective therapies or hospitalizations related to mental health issues
Children with a dissociation disorder may:
- Feel somewhat outside
- Keep staring out the window.
- Keep a secret circle of imaginary buddies
- Leave out what they’ve really said or done
- Suffer from Attention Deficit/Hyperactivity Disorder
Diagnosis of Dissociation
During your visit, your doctor will check your vitals and inquire about any history of illness, both mental and physical. Please inform them if you are in the process of taking any prescription or illegal substances. If they suspect that a medical issue is to blame for your dissociation, they may take a blood sample or do additional tests to rule it out. To rule out certain seizure diseases, which may sometimes induce dissociation, they may also prescribe an electroencephalogram (EEG), a painless test that analyzes brain waves.
A referral to a mental health expert may then be made by your primary care physician. A psychiatric social worker, psychologist, or psychiatrist may be able to help you. Any traumatic experiences you may have had in the past may be of interest to them.
Additional tests may be performed, such as:
- Dissociative Experiences Scale (DES)
- Structured Clinical Interview for Dissociation
Treatment for Dissociation
Although there is currently no cure for dissociation, some people have found relief with a combination of medicine and therapy. The severity and origin of your symptoms will determine how your doctor treats you.
We may prescribe the following medications to you:
Psychotherapy:
You may be able to identify what’s triggering your dissociation with this form of therapy. The objective is to alleviate or at least control your symptoms.
Some examples of psychotherapies are:
- Cognitive behavioral therapy: The goal is to assist you in recognizing and altering unhelpful ways of thinking and behaving.
- Hypnotherapy: When you’re at ease, you could discover that your memories are simpler to uncover and analyze. This should only be done by a hypnotist with expertise in dissociative disorders and post-traumatic stress disorder.
- Phasic trauma treatment: Stopping suicidal thoughts or self-destructive conduct is the primary goal of this therapy. Your psychotherapist will next guide you step-by-step as you go through any painful memories and, if required, reintegrate your identities..
- Family treatment: Having someone you care about there for you, like a spouse or partner, may be a huge benefit.
- Dialectical behavioral therapy: You could find that it teaches you how to manage your emotions and put a halt to destructive habits. Borderline personality disorder is often treated in this way.
- Eye movement desensitization and reprocessing: For the purpose of processing traumatic memories, it incorporates visual exercises and strategies from cognitive behavioral therapy. It has the potential to alleviate PTSD symptoms such as nightmares and flashbacks.
Add-on medication
If you’re having trouble sleeping or dealing with worry, your doctor may prescribe medication, such as antidepressants or a mood stabilizer. You could need an antipsychotic medication if you suffer from schizophrenia.
A Note from Known_Psychology
One of the most common ways that people with C-PTSD and related conditions engage in dissociation, is to dissociate their thoughts from their own thoughts, experience their identity as more of a collection of body parts that they are monitoring green screen, out of frame, and from the other side of a time delay, have consciousness, and store and/or recall memories.
Known_Psychology aims to bring back to light, and those resources that we provide to those who face or know the faces of these challenges. Dissociation and the ability to other ourselves can be triggered by trauma, or used as a coping mechanism, but the differences in manifestations is incredibly important in managing and healing. We want to be able to provide a complete piece, where we explore the root causes and symptoms that comes with it, for individuals to better understand what and how they are dealing with it. Come with us as we explore psychology further and create a community of increased awareness and empathy.
References
Richard J. Loewenstein, senior psychiatrist; medical director, The Trauma Disorders Program, Sheppard Pratt Health System; clinical professor of psychiatry, University of Maryland Medical School.
- Acta Obstetricia et Gynecologica Scandinavica: “Tonic immobility during sexual assault — a common reaction predicting post-traumatic stress disorder and severe depression.”
- American Journal of Psychiatry: “Symptoms of dissociation in humans experiencing acute, uncontrollable stress: a prospective investigation.”
- American Psychiatric Association: “What are Dissociative Disorders?”
- Archives of Neuropsychiatry: “The Relationships Between Dissociation, Attention, and Memory Dysfunction.
- Clinical Psychopharmacology and Neuroscience: “The Many Faces of Dissociation: Opportunities for Innovative Research in Psychiatry.”
- Cleveland Clinic: “Dissociative Identity Disorder (Multiple Personality Disorder): Diagnosis and Tests; Management and Treatment.”
- Culture, Medicine, and Psychiatry: Dissociative Experience and Cultural Neuroscience: Narrative, Metaphor and Mechanism.”
- Dialogues in Clinical Neuroscience: “Dissociation debates: everything you know is wrong.”
- European Journal of Psychotraumatology: “Trauma-related dissociation and altered states of consciousness: a call for clinical, treatment, and neuroscience research.”
- Frontiers in Psychology: “Psychedelics, Meditation, and Self-Consciousness.”
- Journal of Family Violence: “The Role of Dissociation in the Cycle of Violence.”
- Journal of Traumatic Stress: The Association Between Peritraumatic Dissociation and PTSD Symptoms: The Mediating Role of Negative Beliefs About the Self.”
- National Alliance on Mental Illness: “Dissociative Disorders.”
- National Health Service (UK): “Dissociative disorders.”
- Neuroscience of Consciousness: “Dimensions of consciousness and the psychedelic state.”
- Neuropsychiatric Disease and Treatment: “Dissociation in schizophrenia and borderline personality disorder.”
- Sheppard Pratt Health System: “Dissociative Identity Disorder (DID).”
- The American Journal of Psychiatry: “Dissociation in Psychiatric Disorders: A Meta-Analysis of Studies Using the Dissociative Experiences Scale.”
- World Psychiatry: “Recent developments in the theory of dissociation.”
Mariam holds an MS in Sociology with a specialization in Medical Sociology and Social Psychology. With a strong academic background and extensive research work in both fields, she brings depth and clarity to complex topics. Her writing explores the intersection of society, health, and the human mind, making academic ideas easy to grasp and relevant to everyday life.

onlinecanadianpharmacy 24: Express Canada Pharm – escrow pharmacy canada
https://expresscanadapharm.com/# Express Canada Pharm
canadian pharmacy meds review: Express Canada Pharm – cheapest pharmacy canada
Express Canada Pharm canadian pharmacy store Express Canada Pharm
Express Canada Pharm: canadian drug – canada pharmacy online legit
https://expresscanadapharm.shop/# Express Canada Pharm
legitimate canadian pharmacy: canadian pharmacy world – canadian drug
Express Canada Pharm canadian pharmacy no scripts canadian drug stores
reliable canadian online pharmacy: canadian pharmacy ltd – Express Canada Pharm
https://expresscanadapharm.shop/# real canadian pharmacy
Express Canada Pharm: Express Canada Pharm – Express Canada Pharm
Express Canada Pharm: safe reliable canadian pharmacy – Express Canada Pharm
the canadian pharmacy: Express Canada Pharm – legitimate canadian pharmacy online
https://expresscanadapharm.shop/# canadian pharmacy meds reviews
Express Canada Pharm canada cloud pharmacy my canadian pharmacy review
safe canadian pharmacy: canadian pharmacies – Express Canada Pharm
Express Canada Pharm: Express Canada Pharm – Express Canada Pharm
http://expresscanadapharm.com/# best canadian pharmacy to buy from
Express Canada Pharm: canada pharmacy online legit – canadian pharmacy tampa
legit canadian pharmacy online: Express Canada Pharm – Express Canada Pharm
https://expresscanadapharm.shop/# Express Canada Pharm
pharmacy in canada: canadian pharmacy online ship to usa – Express Canada Pharm
canadian mail order pharmacy: canadian pharmacies that deliver to the us – Express Canada Pharm
mexican pharmacy online Cert Pharm Cert Pharm
https://certpharm.com/# mexican pharmacy online
Mexican Cert Pharm: Legit online Mexican pharmacy – Mexican Cert Pharm
https://certpharm.com/# Legit online Mexican pharmacy
Legit online Mexican pharmacy: buying prescription drugs in mexico – buying prescription drugs in mexico
buying from online mexican pharmacy https://certpharm.shop/# mexican pharmacy online
Cert Pharm mexican pharmacy online Best Mexican pharmacy online
https://certpharm.shop/# Best Mexican pharmacy online
Best Mexican pharmacy online: mexican pharmacy online – mexican pharmacy online
buying prescription drugs in mexico https://certpharm.com/# Best Mexican pharmacy online
mexican pharmacy: mexican pharmacy – Mexican Cert Pharm
http://certpharm.com/# Mexican Cert Pharm
Best Mexican pharmacy online: buying prescription drugs in mexico – mexican pharmacy
Cert Pharm Mexican Cert Pharm mexican pharmacy online
Best Mexican pharmacy online: Mexican Cert Pharm – Legit online Mexican pharmacy
https://certpharm.com/# buying prescription drugs in mexico online
Legit online Mexican pharmacy: mexican pharmacy online – Mexican Cert Pharm
http://certpharm.com/# Mexican Cert Pharm
mexican pharmacy online Mexican Cert Pharm Legit online Mexican pharmacy
Mexican Cert Pharm: mexican pharmacy online – mexican drugstore online
pharmacies in mexico that ship to usa https://certpharm.com/# Best Mexican pharmacy online
mexican pharmacy online: п»їbest mexican online pharmacies – Mexican Cert Pharm
https://certpharm.com/# Cert Pharm
Best Mexican pharmacy online: Cert Pharm – Best Mexican pharmacy online
buying prescription drugs in mexico Best Mexican pharmacy online mexican pharmacy
https://certpharm.shop/# Cert Pharm
mexican pharmacy online: Best Mexican pharmacy online – Legit online Mexican pharmacy
mexican drugstore online: Best Mexican pharmacy online – mexican pharmacy
mexico drug stores pharmacies http://certpharm.com/# Mexican Cert Pharm
mexican pharmacy: Mexican Cert Pharm – Best Mexican pharmacy online
https://certpharm.com/# buying prescription drugs in mexico online
mexican pharmacy online: mexico drug stores pharmacies – mexican pharmacy online
mexican pharmacy Legit online Mexican pharmacy mexican border pharmacies shipping to usa
http://plinkocasi.com/# Plinko games
plinko ball: plinko fr – plinko
https://plinkofr.com/# plinko game
Plinko game: Plinko game – Plinko online game
plinko: plinko nl – plinko casino nederland
https://plinkocasi.com/# Plinko casino game
plinko casino plinko game PlinkoFr
plinko: plinko fr – plinko argent reel avis
plinko ball: PlinkoDeutsch – PlinkoDeutsch
plinko france: plinko casino – PlinkoFr
https://plinkocasinonl.com/# plinko spelen
Plinko-game Plinko online game Plinko games
pinco slot: pinco.legal – pinco.legal
https://plinkocasinonl.com/# plinko nederland
https://plinkodeutsch.shop/# plinko wahrscheinlichkeit
plinko nl: plinko – plinko casino
plinko argent reel avis: plinko casino – plinko argent reel avis
http://plinkocasinonl.com/# plinko nederland
plinko betrouwbaar: plinko nl – plinko casino nederland
https://plinkocasinonl.shop/# plinko nederland
plinko: plinko casino – plinko betrouwbaar
plinko: plinko wahrscheinlichkeit – PlinkoDeutsch
http://plinkocasinonl.com/# plinko nederland
Plinko games: Plinko app – Plinko
plinko casino: plinko casino – plinko spelen
https://plinkodeutsch.com/# plinko germany
Plinko game for real money: Plinko online game – Plinko online game
pinco.legal: pinco slot – pinco.legal
https://plinkodeutsch.com/# plinko wahrscheinlichkeit
https://pinco.legal/# pinco.legal
plinko france plinko plinko argent reel avis
pinco casino: pinco casino – pinco slot
pinco slot: pinco.legal – pinco casino
Plinko casino game: Plinko online game – Plinko games
plinko france plinko game PlinkoFr
Plinko casino game: Plinko-game – Plinko-game
plinko game: plinko erfahrung – Plinko Deutsch
http://plinkofr.com/# plinko game
plinko erfahrung: plinko ball – plinko geld verdienen
https://plinkofr.com/# plinko argent reel avis
pinco casino: pinco casino – pinco slot
plinko spelen: plinko nederland – plinko casino
plinko erfahrung plinko ball Plinko Deutsch
http://plinkodeutsch.com/# Plinko Deutsch
pinco: pinco.legal – pinco casino
Plinko game for real money: Plinko-game – Plinko online game
https://pinco.legal/# pinco
plinko spelen: plinko – plinko nederland
plinko: plinko fr – plinko casino
https://plinkocasi.com/# Plinko app
plinko casino: plinko fr – plinko
pinco slot pinco pinco
pinco casino: pinco casino – pinco legal
https://plinkofr.com/# plinko casino
plinko erfahrung: PlinkoDeutsch – plinko geld verdienen
https://pinco.legal/# pinco casino
PlinkoFr: plinko – avis plinko
https://pinco.legal/# pinco slot
plinko casino nederland: plinko spelen – plinko casino nederland
Plinko online game: Plinko casino game – Plinko app
plinko casino: plinko nederland – plinko spelen
https://plinkocasinonl.shop/# plinko casino nederland
plinko nl: plinko nl – plinko nl
http://pinco.legal/# pinco slot
Plinko Deutsch: plinko casino – plinko wahrscheinlichkeit
plinko plinko game avis plinko
plinko spelen: plinko betrouwbaar – plinko spelen
pinco.legal: pinco.legal – pinco legal
https://plinkocasinonl.shop/# plinko casino nederland
pinco.legal: pinco casino – pinco casino
Plinko casino game Plinko app Plinko game
https://plinkocasi.com/# Plinko
plinko argent reel avis: avis plinko – plinko
https://plinkocasi.com/# Plinko online
pharmacie en ligne france pas cher https://pharmaciemeilleurprix.shop/# Pharmacie sans ordonnance
https://viagrameilleurprix.com/# Viagra pas cher paris
pharmacie en ligne sans ordonnance
Здесь можно узнать способы диагностики и подходы по восстановлению.
http://clearapplications.com/__media__/js/netsoltrademark.php?d=empathycenter.ru%2Fpreparations%2Fo%2Fokskarbazepin%2F
Отдельный раздел уделяется психологическим особенностям и их влиянию на психическим здоровьем.
Также рассматриваются современные терапевтические и психологические методы лечения.
Материалы помогут разобраться, как правильно подходить к угнетенным состоянием в пожилом возрасте.
Viagra vente libre allemagne viagra en ligne Viagra homme prix en pharmacie
https://viagrameilleurprix.com/# Viagra vente libre allemagne
pharmacie en ligne fiable
http://kamagrameilleurprix.com/# Achat mГ©dicament en ligne fiable
pharmacie en ligne fiable
pharmacie en ligne pas cher kamagra en ligne trouver un mГ©dicament en pharmacie
trouver un mГ©dicament en pharmacie https://tadalafilmeilleurprix.com/# pharmacie en ligne livraison europe
На этом сайте АвиаЛавка (AviaLavka) вы можете забронировать выгодные авиабилеты по всему миру.
Мы подбираем лучшие тарифы от проверенных перевозчиков.
Простой интерфейс позволит быстро найти подходящий рейс.
https://www.avialavka.ru
Интеллектуальный фильтр помогает подобрать оптимальные варианты перелетов.
Покупайте билеты в пару кликов без скрытых комиссий.
АвиаЛавка — ваш надежный помощник в путешествиях!
pharmacie en ligne sans ordonnance: pharmacie en ligne france – pharmacie en ligne fiable
https://tadalafilmeilleurprix.shop/# Pharmacie en ligne livraison Europe
Pharmacie Internationale en ligne
pharmacie en ligne france pas cher https://tadalafilmeilleurprix.shop/# Pharmacie en ligne livraison Europe
pharmacie en ligne france livraison internationale Acheter Cialis п»їpharmacie en ligne france
pharmacie en ligne sans ordonnance: kamagra en ligne – pharmacie en ligne avec ordonnance
https://viagrameilleurprix.com/# Viagra prix pharmacie paris
Pharmacie Internationale en ligne
trouver un mГ©dicament en pharmacie: acheter kamagra site fiable – pharmacie en ligne france livraison belgique
https://viagrameilleurprix.com/# SildГ©nafil 100 mg prix en pharmacie en France
pharmacie en ligne pas cher
pharmacie en ligne france pas cher Pharmacie sans ordonnance pharmacie en ligne
pharmacie en ligne livraison europe: Tadalafil sans ordonnance en ligne – pharmacie en ligne pas cher
https://kamagrameilleurprix.shop/# pharmacies en ligne certifiГ©es
acheter mГ©dicament en ligne sans ordonnance
pharmacie en ligne: kamagra livraison 24h – Pharmacie sans ordonnance
Viagra pas cher livraison rapide france Viagra sans ordonnance 24h Viagra gГ©nГ©rique sans ordonnance en pharmacie
http://tadalafilmeilleurprix.com/# Pharmacie sans ordonnance
pharmacie en ligne livraison europe
pharmacie en ligne france fiable: cialis prix – pharmacie en ligne france fiable
Viagra homme sans ordonnance belgique: Viagra sans ordonnance 24h – Prix du Viagra 100mg en France
https://pharmaciemeilleurprix.com/# pharmacie en ligne avec ordonnance
Pharmacie en ligne livraison Europe
pharmacie en ligne france pas cher kamagra en ligne trouver un mГ©dicament en pharmacie
pharmacie en ligne: Cialis sans ordonnance 24h – pharmacie en ligne france fiable
pharmacie en ligne pas cher https://pharmaciemeilleurprix.com/# pharmacie en ligne france fiable
Pharmacie Internationale en ligne: Cialis sans ordonnance 24h – pharmacie en ligne france pas cher
Achat mГ©dicament en ligne fiable: cialis sans ordonnance – pharmacie en ligne france pas cher
Pharmacie Internationale en ligne pharmacie en ligne pas cher trouver un mГ©dicament en pharmacie
https://kamagrameilleurprix.shop/# pharmacie en ligne
pharmacie en ligne avec ordonnance
pharmacie en ligne pas cher: cialis prix – pharmacie en ligne sans ordonnance
vente de mГ©dicament en ligne: cialis prix – Pharmacie sans ordonnance
Sildenafil teva 100 mg sans ordonnance viagra sans ordonnance Viagra sans ordonnance pharmacie France
pharmacie en ligne france pas cher: kamagra gel – pharmacie en ligne fiable
https://tadalafilmeilleurprix.shop/# pharmacie en ligne
Pharmacie en ligne livraison Europe
pharmacie en ligne sans ordonnance: pharmacie en ligne – Achat mГ©dicament en ligne fiable
SildГ©nafil 100 mg prix en pharmacie en France: viagra sans ordonnance – Le gГ©nГ©rique de Viagra
Viagra pas cher inde: Acheter Viagra Cialis sans ordonnance – Acheter Sildenafil 100mg sans ordonnance
https://pharmaciemeilleurprix.shop/# pharmacie en ligne france fiable
pharmacie en ligne pas cher
pharmacie en ligne fiable achat kamagra pharmacie en ligne france livraison internationale
pharmacie en ligne https://kamagrameilleurprix.shop/# pharmacie en ligne avec ordonnance
pharmacie en ligne france livraison belgique: kamagra en ligne – Achat mГ©dicament en ligne fiable
Viagra sans ordonnance 24h Amazon: acheter du viagra – Sildenafil teva 100 mg sans ordonnance
Viagra pas cher inde: Acheter Viagra Cialis sans ordonnance – Quand une femme prend du Viagra homme
https://pharmaciemeilleurprix.com/# Pharmacie en ligne livraison Europe
vente de mГ©dicament en ligne
acheter mГ©dicament en ligne sans ordonnance http://pharmaciemeilleurprix.com/# pharmacie en ligne france fiable
pharmacie en ligne sans ordonnance: cialis generique – pharmacies en ligne certifiГ©es
trouver un mГ©dicament en pharmacie kamagra gel vente de mГ©dicament en ligne
pharmacie en ligne avec ordonnance: pharmacie en ligne france livraison belgique – Pharmacie Internationale en ligne
https://kamagrameilleurprix.shop/# trouver un mГ©dicament en pharmacie
п»їpharmacie en ligne france
Pharmacie Internationale en ligne: pharmacie en ligne pas cher – Pharmacie Internationale en ligne
п»їpharmacie en ligne france: pharmacie en ligne sans ordonnance – Pharmacie Internationale en ligne
acheter mГ©dicament en ligne sans ordonnance http://viagrameilleurprix.com/# Viagra femme ou trouver
http://kamagrameilleurprix.com/# п»їpharmacie en ligne france
vente de mГ©dicament en ligne
Pharmacie Internationale en ligne: pharmacie en ligne pas cher – vente de mГ©dicament en ligne
vente de mГ©dicament en ligne: pharmacie en ligne pas cher – pharmacie en ligne france livraison internationale
pharmacie en ligne fiable https://pharmaciemeilleurprix.shop/# Pharmacie en ligne livraison Europe
pharmacie en ligne pas cher: Tadalafil sans ordonnance en ligne – pharmacie en ligne sans ordonnance
https://pharmaciemeilleurprix.com/# pharmacie en ligne
pharmacie en ligne france pas cher
pharmacies en ligne certifiГ©es: pharmacie en ligne pas cher – pharmacie en ligne avec ordonnance
Viagra Pfizer sans ordonnance: acheter du viagra – Prix du Viagra en pharmacie en France
acheter mГ©dicament en ligne sans ordonnance: pharmacie en ligne pas cher – Pharmacie en ligne livraison Europe
https://tadalafilmeilleurprix.shop/# pharmacie en ligne fiable
acheter mГ©dicament en ligne sans ordonnance
п»їpharmacie en ligne france pharmacie en ligne france pharmacie en ligne
pharmacie en ligne pas cher: kamagra livraison 24h – pharmacie en ligne sans ordonnance
pharmacie en ligne fiable: pharmacie en ligne – Pharmacie en ligne livraison Europe
pharmacie en ligne pas cher https://tadalafilmeilleurprix.shop/# п»їpharmacie en ligne france
pharmacie en ligne: cialis prix – pharmacie en ligne france fiable
acheter mГ©dicament en ligne sans ordonnance: kamagra gel – Pharmacie Internationale en ligne
Viagra 100mg prix: viagra sans ordonnance – Viagra sans ordonnance livraison 48h
Le gГ©nГ©rique de Viagra acheter du viagra Viagra homme prix en pharmacie
https://tadalafilmeilleurprix.shop/# pharmacie en ligne avec ordonnance
trouver un mГ©dicament en pharmacie
pharmacie en ligne france pas cher: pharmacie en ligne – Pharmacie en ligne livraison Europe
pharmacie en ligne: achat kamagra – acheter mГ©dicament en ligne sans ordonnance
acheter mГ©dicament en ligne sans ordonnance: kamagra en ligne – acheter mГ©dicament en ligne sans ordonnance
https://pharmaciemeilleurprix.shop/# vente de mГ©dicament en ligne
Pharmacie Internationale en ligne
Viagra gГ©nГ©rique sans ordonnance en pharmacie: acheter du viagra – Viagra pas cher inde
vente de mГ©dicament en ligne: pharmacie en ligne sans ordonnance – Pharmacie Internationale en ligne
Viagra homme sans prescription acheter du viagra SildГ©nafil 100 mg prix en pharmacie en France
Pharmacie sans ordonnance https://kamagrameilleurprix.shop/# pharmacie en ligne sans ordonnance
pharmacies en ligne certifiГ©es: Pharmacie sans ordonnance – pharmacie en ligne sans ordonnance
pharmacie en ligne pas cher https://pharmaciemeilleurprix.shop/# pharmacie en ligne france fiable
Le gГ©nГ©rique de Viagra: Viagra sans ordonnance 24h – Viagra homme sans ordonnance belgique
pharmacie en ligne avec ordonnance: pharmacie en ligne sans ordonnance – pharmacie en ligne france pas cher
http://pharmaciemeilleurprix.com/# pharmacie en ligne avec ordonnance
acheter mГ©dicament en ligne sans ordonnance
pharmacies en ligne certifiГ©es Acheter Cialis Pharmacie en ligne livraison Europe
acheter mГ©dicament en ligne sans ordonnance: pharmacie en ligne france – pharmacie en ligne sans ordonnance
pharmacie en ligne sans ordonnance https://kamagrameilleurprix.shop/# vente de mГ©dicament en ligne
pharmacie en ligne avec ordonnance: acheter kamagra site fiable – vente de mГ©dicament en ligne
pharmacie en ligne: pharmacie en ligne pas cher – pharmacie en ligne fiable
http://pharmaciemeilleurprix.com/# pharmacie en ligne france livraison internationale
Pharmacie Internationale en ligne
trouver un mГ©dicament en pharmacie https://kamagrameilleurprix.shop/# pharmacie en ligne sans ordonnance
Achat mГ©dicament en ligne fiable Pharmacie sans ordonnance pharmacies en ligne certifiГ©es
acheter mГ©dicament en ligne sans ordonnance: Tadalafil sans ordonnance en ligne – pharmacie en ligne fiable
http://kamagrameilleurprix.com/# pharmacie en ligne fiable
Pharmacie Internationale en ligne
trouver un mГ©dicament en pharmacie: kamagra en ligne – pharmacie en ligne avec ordonnance
п»їpharmacie en ligne france: pharmacie en ligne – pharmacie en ligne france livraison internationale
Achat mГ©dicament en ligne fiable: cialis prix – pharmacie en ligne pas cher
http://pharmaciemeilleurprix.com/# trouver un mГ©dicament en pharmacie
pharmacie en ligne livraison europe
Pharmacie sans ordonnance https://tadalafilmeilleurprix.shop/# pharmacies en ligne certifiГ©es
Viagra sans ordonnance livraison 24h Viagra sans ordonnance 24h Viagra gГ©nГ©rique sans ordonnance en pharmacie
pharmacie en ligne france pas cher: pharmacie en ligne avec ordonnance – pharmacie en ligne france livraison internationale
Viagra sans ordonnance 24h suisse: viagra en ligne – Viagra sans ordonnance pharmacie France
https://kamagrameilleurprix.com/# pharmacie en ligne sans ordonnance
Pharmacie Internationale en ligne
vente de mГ©dicament en ligne: Pharmacies en ligne certifiees – Pharmacie en ligne livraison Europe
Pharmacie sans ordonnance: acheter kamagra site fiable – Pharmacie en ligne livraison Europe
https://kamagrameilleurprix.com/# Pharmacie Internationale en ligne
pharmacie en ligne france fiable
pharmacie en ligne france fiable pharmacie en ligne pharmacie en ligne france fiable
п»їpharmacie en ligne france: kamagra gel – Pharmacie sans ordonnance
http://viagrameilleurprix.com/# Viagra gГ©nГ©rique pas cher livraison rapide
pharmacie en ligne livraison europe
pharmacie en ligne france fiable https://tadalafilmeilleurprix.com/# pharmacie en ligne france pas cher
pharmacie en ligne avec ordonnance: pharmacie en ligne france – pharmacie en ligne france pas cher
pharmacie en ligne: cialis generique – pharmacie en ligne fiable
pharmacie en ligne avec ordonnance pharmacie en ligne sans ordonnance pharmacie en ligne pas cher
trouver un mГ©dicament en pharmacie: Pharmacie sans ordonnance – pharmacie en ligne fiable
https://kamagrameilleurprix.shop/# pharmacie en ligne france pas cher
pharmacie en ligne avec ordonnance
acheter mГ©dicament en ligne sans ordonnance: pharmacie en ligne pas cher – acheter mГ©dicament en ligne sans ordonnance
pharmacie en ligne france livraison internationale https://kamagrameilleurprix.shop/# pharmacie en ligne avec ordonnance
order cheap clomid pills: clomid without a prescription – how to buy generic clomid without prescription
where buy generic clomid without rx clomid brand name cost clomid without insurance
amoxicillin 800 mg price: Amo Health Pharm – where can i buy amoxocillin
doxycycline 200 mg capsules: doxycycline tablets 100mg – doxycycline online with no prescription
https://doxhealthpharm.shop/# buy vibramycin
zithromax capsules: Zithro Pharm – zithromax online pharmacy canada
where buy generic clomid pill: where buy generic clomid price – where can i get cheap clomid
how to get clomid no prescription: ClmHealthPharm – where buy cheap clomid without dr prescription
doxycycline order online uk Dox Health Pharm doxycycline 75 mg
where to buy generic clomid without prescription: ClmHealthPharm – how to buy clomid for sale
amoxicillin 500mg capsule buy online: amoxicillin 500 mg price – amoxicillin generic
doxycycline 50 mg: doxycycline tablet – doxycycline generic price
doxycycline capsules 40 mg: DoxHealthPharm – doxycycline gel
cost cheap clomid online: can i order generic clomid without dr prescription – can i order generic clomid tablets
doxycycline prescription uk: doxycycline for sale uk – how to get doxycycline
https://doxhealthpharm.com/# doxycycline order online
where to buy amoxicillin 500mg without prescription Amo Health Pharm amoxicillin no prescipion
can i buy doxycycline over the counter uk: how to order doxycycline – doxycycline 150 mg tablets
buy cheap amoxicillin online: generic amoxicillin cost – generic amoxicillin 500mg
where to buy amoxicillin over the counter: where to get amoxicillin over the counter – amoxicillin azithromycin
500 mg doxycycline pill: Dox Health Pharm – how can i get doxycycline
zithromax buy online: Zithro Pharm – zithromax prescription in canada
how to get zithromax online: where can i buy zithromax capsules – buy zithromax online cheap
where to buy amoxicillin: Amo Health Pharm – amoxicillin over counter
price of doxycycline 100mg in india Dox Health Pharm doxycycline 50 medicine
can i get generic clomid online: ClmHealthPharm – get clomid
zithromax 500 mg: Zithro Pharm – zithromax antibiotic without prescription
can i purchase cheap clomid: where to get generic clomid price – how to buy clomid without rx
amoxicillin canada price over the counter amoxicillin amoxicillin pills 500 mg
zithromax pill: Zithro Pharm – zithromax
cost doxycycline 100mg: cost of doxycycline canada – where can i get doxycycline over the counter
https://clmhealthpharm.shop/# can you buy cheap clomid without dr prescription
buy zithromax without presc: ZithroPharm – where can i purchase zithromax online
doxycycline australia: doxycycline capsules purchase – doxycycline over the counter south africa
can you buy doxycycline over the counter canada: Dox Health Pharm – doxycycline canada pharmacy
amoxicillin over the counter in canada: purchase amoxicillin online – amoxicillin brand name
amoxicillin 500mg capsules uk: canadian pharmacy amoxicillin – amoxicillin 500 mg tablet price
doxycycline 50mg tablets price Dox Health Pharm doxycycline cheap uk
doxycycline iv: doxycycline mono – doxycycline 2984
doxycycline 100mg capsule sale: cost doxycycline 100mg – doxycycline medication
zithromax capsules 250mg: ZithroPharm – zithromax 500 mg lowest price pharmacy online
cost cheap clomid without dr prescription: can i order clomid tablets – cheap clomid now
zithromax price south africa: purchase zithromax online – buy zithromax no prescription
amoxicillin cost australia: buy amoxicillin online cheap – where to buy amoxicillin pharmacy
amoxicillin cost australia amoxicillin 500mg buy online uk buy amoxicillin online mexico
get generic clomid price: where buy clomid price – get cheap clomid without rx
where buy clomid prices: ClmHealthPharm – cheap clomid without a prescription
over the counter amoxicillin canada: buy amoxicillin 500mg canada – amoxicillin capsule 500mg price
Pemain harus menetapkan batas saat bermain https://slotdemo.auction/# Slot memberikan kesempatan untuk menang besar
Mesin slot menawarkan berbagai tema menarik: slot88.company – slot88.company
Banyak pemain menikmati jackpot harian di slot http://bonaslot.site/# п»їKasino di Indonesia sangat populer di kalangan wisatawan
BonaSlot bonaslot Mesin slot sering diperbarui dengan game baru
Kasino menawarkan pengalaman bermain yang seru http://garuda888.top/# Banyak pemain berusaha untuk mendapatkan jackpot
Kasino di Jakarta memiliki berbagai pilihan permainan: bonaslot – bonaslot
Mesin slot digital semakin banyak diminati https://garuda888.top/# Kasino selalu memperbarui mesin slotnya
Banyak pemain berusaha untuk mendapatkan jackpot https://garuda888.top/# Kasino di Bali menarik banyak pengunjung
http://garuda888.top/# Slot dengan tema budaya lokal menarik perhatian
Pemain sering mencoba berbagai jenis slot: bonaslot – bonaslot.site
preman69.tech preman69.tech Kasino di Indonesia menyediakan hiburan yang beragam
Kasino di Indonesia menyediakan hiburan yang beragam http://garuda888.top/# Slot memberikan kesempatan untuk menang besar
https://slot88.company/# Kasino mendukung permainan bertanggung jawab
Mesin slot sering diperbarui dengan game baru: preman69.tech – preman69.tech
Slot modern memiliki grafik yang mengesankan https://bonaslot.site/# Kasino di Jakarta memiliki berbagai pilihan permainan
https://slotdemo.auction/# Banyak pemain mencari mesin dengan RTP tinggi
Permainan slot mudah dipahami dan menyenangkan: bonaslot – bonaslot
garuda888 garuda888 slot Pemain harus memahami aturan masing-masing mesin
Kasino memastikan keamanan para pemain dengan baik http://bonaslot.site/# Slot memberikan kesempatan untuk menang besar
На этом сайте вы можете приобрести виртуальные телефонные номера различных операторов. Эти номера могут использоваться для регистрации аккаунтов в различных сервисах и приложениях.
В каталоге представлены как долговременные, так и одноразовые номера, что можно использовать для получения SMS. Это удобное решение для тех, кто не хочет указывать основной номер в сети.
немецкий номер телефона
Процесс покупки очень удобный: выбираете необходимый номер, вносите оплату, и он будет готов к использованию. Попробуйте услугу уже сегодня!
https://garuda888.top/# Mesin slot sering diperbarui dengan game baru
Banyak pemain berusaha untuk mendapatkan jackpot: preman69.tech – preman69.tech
Pemain harus memahami aturan masing-masing mesin https://bonaslot.site/# Slot dengan tema film terkenal menarik banyak perhatian
https://slot88.company/# Slot modern memiliki grafik yang mengesankan
Slot klasik tetap menjadi favorit banyak orang: preman69 slot – preman69 slot
Pemain harus memahami aturan masing-masing mesin http://preman69.tech/# Banyak pemain mencari mesin dengan RTP tinggi
slotdemo akun demo slot Beberapa kasino memiliki area khusus untuk slot
Mesin slot menawarkan pengalaman bermain yang cepat: garuda888.top – garuda888.top
Mesin slot menawarkan pengalaman bermain yang cepat http://garuda888.top/# Slot menjadi bagian penting dari industri kasino
Keseruan bermain slot selalu menggoda para pemain https://slotdemo.auction/# Banyak kasino menawarkan permainan langsung yang seru
Jackpot besar bisa mengubah hidup seseorang: preman69.tech – preman69
Slot dengan pembayaran tinggi selalu diminati http://preman69.tech/# Keseruan bermain slot selalu menggoda para pemain
slot88.company slot88.company Kasino menawarkan pengalaman bermain yang seru
Slot modern memiliki grafik yang mengesankan: slot88.company – slot88.company
http://preman69.tech/# Mesin slot dapat dimainkan dalam berbagai bahasa
Slot dengan bonus putaran gratis sangat populer https://garuda888.top/# Jackpot progresif menarik banyak pemain
Slot dengan pembayaran tinggi selalu diminati: slot 88 – slot88
Kasino menyediakan layanan pelanggan yang baik https://slot88.company/# Kasino memastikan keamanan para pemain dengan baik
https://slotdemo.auction/# Keseruan bermain slot selalu menggoda para pemain
bonaslot.site bonaslot.site Pemain bisa menikmati slot dari kenyamanan rumah
Permainan slot bisa dimainkan dengan berbagai taruhan https://preman69.tech/# Kasino di Jakarta memiliki berbagai pilihan permainan
https://slotdemo.auction/# Pemain harus menetapkan batas saat bermain
Mesin slot baru selalu menarik minat: slot 88 – slot 88
Banyak kasino menawarkan permainan langsung yang seru http://preman69.tech/# Slot dengan pembayaran tinggi selalu diminati
https://preman69.tech/# Slot dengan tema budaya lokal menarik perhatian
Slot menjadi bagian penting dari industri kasino: bonaslot – bonaslot.site
Slot menawarkan berbagai jenis permainan bonus https://bonaslot.site/# Kasino menawarkan pengalaman bermain yang seru
slot 88 slot88 Slot dengan tema film terkenal menarik banyak perhatian
https://slotdemo.auction/# Beberapa kasino memiliki area khusus untuk slot
Slot dengan grafis 3D sangat mengesankan http://garuda888.top/# Banyak pemain mencari mesin dengan RTP tinggi
Slot modern memiliki grafik yang mengesankan: slot88.company – slot 88
https://slotdemo.auction/# Banyak pemain menikmati jackpot harian di slot
Pemain bisa menikmati slot dari kenyamanan rumah http://slot88.company/# Banyak pemain mencari mesin dengan RTP tinggi
Kasino di Jakarta memiliki berbagai pilihan permainan https://slotdemo.auction/# Kasino selalu memperbarui mesin slotnya
Slot dengan fitur interaktif semakin banyak tersedia: slot demo pg gratis – slot demo rupiah
preman69.tech preman69.tech Keseruan bermain slot selalu menggoda para pemain
Slot dengan tema film terkenal menarik banyak perhatian http://slotdemo.auction/# Slot menjadi daya tarik utama di kasino
Jackpot progresif menarik banyak pemain: slot demo rupiah – akun demo slot
Banyak kasino memiliki promosi untuk slot http://slotdemo.auction/# Kasino memastikan keamanan para pemain dengan baik
http://slotdemo.auction/# Mesin slot digital semakin banyak diminati
slot88.company slot88 Bermain slot bisa menjadi pengalaman sosial
Banyak pemain berusaha untuk mendapatkan jackpot: preman69 slot – preman69
Kasino menyediakan layanan pelanggan yang baik https://slotdemo.auction/# Slot dengan tema budaya lokal menarik perhatian
http://bonaslot.site/# Slot menawarkan berbagai jenis permainan bonus
Mesin slot sering diperbarui dengan game baru http://bonaslot.site/# Pemain harus memahami aturan masing-masing mesin
Slot menjadi bagian penting dari industri kasino: slot88.company – slot 88
Bermain slot bisa menjadi pengalaman sosial https://garuda888.top/# Keseruan bermain slot selalu menggoda para pemain
https://bonaslot.site/# Slot dengan bonus putaran gratis sangat populer
bonaslot bonaslot.site Banyak kasino memiliki program loyalitas untuk pemain
Pemain bisa menikmati slot dari kenyamanan rumah https://slotdemo.auction/# Kasino menawarkan pengalaman bermain yang seru
Slot menjadi daya tarik utama di kasino: preman69 – preman69.tech
Kasino memiliki suasana yang energik dan menyenangkan https://bonaslot.site/# Slot menawarkan berbagai jenis permainan bonus
https://slotdemo.auction/# Mesin slot digital semakin banyak diminati
Banyak kasino memiliki promosi untuk slot https://garuda888.top/# Slot dengan tema budaya lokal menarik perhatian
Kasino di Jakarta memiliki berbagai pilihan permainan http://preman69.tech/# Banyak kasino memiliki program loyalitas untuk pemain
Permainan slot bisa dimainkan dengan berbagai taruhan: preman69 slot – preman69.tech
canada pharmacy online trustworthy canadian pharmacy canadian online pharmacy
pharmacy coupons https://xxlmexicanpharm.shop/# xxl mexican pharm
promo code for canadian pharmacy meds https://megaindiapharm.com/# MegaIndiaPharm
mexico drug stores pharmacies: xxl mexican pharm – reputable mexican pharmacies online
best canadian pharmacy no prescription https://familypharmacy.company/# Best online pharmacy
cheapest pharmacy to get prescriptions filled https://discountdrugmart.pro/# discount drug mart pharmacy
easy canadian pharm: canadianpharmacymeds – canadian pharmacy online ship to usa
buying prescription drugs from canada https://megaindiapharm.com/# top online pharmacy india
no prescription needed canadian pharmacy https://megaindiapharm.shop/# MegaIndiaPharm
MegaIndiaPharm Mega India Pharm Mega India Pharm
online pharmacy india: MegaIndiaPharm – MegaIndiaPharm
pharmacy without prescription https://megaindiapharm.com/# Mega India Pharm
non prescription medicine pharmacy https://xxlmexicanpharm.com/# mexico drug stores pharmacies
Online medicine order: Online medicine home delivery – Mega India Pharm
online pharmacy non prescription drugs: online pharmacy delivery usa – Cheapest online pharmacy
drugstore com online pharmacy prescription drugs https://easycanadianpharm.com/# easy canadian pharm
us pharmacy no prescription http://discountdrugmart.pro/# discount drugs
discount drug pharmacy discount drug mart pharmacy drug mart
rx pharmacy no prescription https://easycanadianpharm.com/# easy canadian pharm
family pharmacy: canadian pharmacy world coupon – pharmacy discount coupons
us pharmacy no prescription http://discountdrugmart.pro/# prescription drugs online
us pharmacy no prescription http://xxlmexicanpharm.com/# best online pharmacies in mexico
Best online pharmacy: Online pharmacy USA – Best online pharmacy
canadian pharmacies not requiring prescription https://xxlmexicanpharm.shop/# mexico drug stores pharmacies
easy canadian pharm easy canadian pharm easy canadian pharm
canadian online pharmacy no prescription http://familypharmacy.company/# Online pharmacy USA
pharmacies in mexico that ship to usa: xxl mexican pharm – xxl mexican pharm
best no prescription pharmacy http://discountdrugmart.pro/# discount drug pharmacy
online pharmacy without prescription https://discountdrugmart.pro/# discount drug pharmacy
mexico drug stores pharmacies: mexico pharmacies prescription drugs – xxl mexican pharm
pharmacy website india Mega India Pharm best india pharmacy
canadian pharmacy world coupon https://familypharmacy.company/# Cheapest online pharmacy
cheapest pharmacy for prescriptions without insurance https://familypharmacy.company/# Online pharmacy USA
drugmart: discount drug mart pharmacy – canadian prescription pharmacy
Best online pharmacy: online pharmacy delivery usa – us pharmacy no prescription
canadian prescription pharmacy https://easycanadianpharm.com/# easy canadian pharm
online pharmacy discount code https://xxlmexicanpharm.com/# mexican rx online
mexican drugstore online: mexican online pharmacies prescription drugs – best online pharmacies in mexico
pharmacy no prescription required https://familypharmacy.company/# Online pharmacy USA
canada rx pharmacy easy canadian pharm easy canadian pharm
discount drug pharmacy: discount drug pharmacy – drugmart
cheap pharmacy no prescription http://megaindiapharm.com/# online shopping pharmacy india
MegaIndiaPharm: best india pharmacy – MegaIndiaPharm
no prescription required pharmacy https://easycanadianpharm.com/# easy canadian pharm
purple pharmacy mexico price list: xxl mexican pharm – xxl mexican pharm
canadian pharmacy world coupons http://easycanadianpharm.com/# best canadian pharmacy
canadian online pharmacy no prescription https://familypharmacy.company/# Online pharmacy USA
drugmart: discount drug mart pharmacy – discount drug pharmacy
easy canadian pharm canadian drugs pharmacy canadian pharmacy ltd
pharmacy online 365 discount code https://easycanadianpharm.com/# easy canadian pharm
online pharmacy india: Mega India Pharm – MegaIndiaPharm
offshore pharmacy no prescription https://familypharmacy.company/# Online pharmacy USA
MegaIndiaPharm: MegaIndiaPharm – Mega India Pharm
canadian pharmacy discount code https://xxlmexicanpharm.com/# reputable mexican pharmacies online
discount drug pharmacy: pharmacy coupons – discount drug mart
canadian pharmacy discount code https://xxlmexicanpharm.com/# xxl mexican pharm
mexico pharmacies prescription drugs xxl mexican pharm medication from mexico pharmacy
Best online pharmacy: online pharmacy delivery usa – online pharmacy delivery usa
legal online pharmacy coupon code https://discountdrugmart.pro/# discount drugs
overseas pharmacy no prescription https://easycanadianpharm.com/# easy canadian pharm
discount drug mart pharmacy: discount drug mart – discount drugs
Cheapest online pharmacy: Best online pharmacy – Best online pharmacy
canadian pharmacies not requiring prescription http://xxlmexicanpharm.com/# buying from online mexican pharmacy
online shopping pharmacy india: Mega India Pharm – Online medicine home delivery
Cheapest online pharmacy online pharmacy delivery usa Cheapest online pharmacy
cheapest pharmacy to get prescriptions filled http://discountdrugmart.pro/# discount drugs
non prescription medicine pharmacy https://discountdrugmart.pro/# discount drug mart pharmacy
online pharmacy non prescription drugs http://xxlmexicanpharm.com/# xxl mexican pharm
xxl mexican pharm: mexican online pharmacies prescription drugs – xxl mexican pharm
family pharmacy: Best online pharmacy – Cheapest online pharmacy
Online pharmacy USA family pharmacy Online pharmacy USA
canada drugs coupon code https://discountdrugmart.pro/# discount drugs
drug mart: drugmart – discount drug mart pharmacy
promo code for canadian pharmacy meds https://xxlmexicanpharm.com/# xxl mexican pharm
canadian pharmacy coupon https://familypharmacy.company/# family pharmacy
easy canadian pharm: canadian pharmacy meds review – easy canadian pharm
mail order pharmacy india: indian pharmacy paypal – MegaIndiaPharm
Best online pharmacy Best online pharmacy Online pharmacy USA
canadian pharmacy coupon https://xxlmexicanpharm.com/# best online pharmacies in mexico
legal online pharmacy coupon code https://discountdrugmart.pro/# drug mart
xxl mexican pharm: xxl mexican pharm – xxl mexican pharm
mexico pharmacies prescription drugs: mexico drug stores pharmacies – pharmacies in mexico that ship to usa
canadian online pharmacy no prescription https://xxlmexicanpharm.shop/# buying from online mexican pharmacy
cheapest pharmacy prescription drugs http://megaindiapharm.com/# Mega India Pharm
easy canadian pharm: canadian pharmacy drugs online – easy canadian pharm
canadian pharmacy no prescription needed https://xxlmexicanpharm.com/# xxl mexican pharm
Mega India Pharm MegaIndiaPharm Mega India Pharm
https://jugabet.xyz/# Las reservas en lГnea son fГЎciles y rГЎpidas.
Players enjoy both fun and excitement in casinos.
Security measures ensure a safe environment. https://phmacao.life/# Casinos often host special holiday promotions.
taya777 login taya777 register login Many casinos provide shuttle services for guests.
Gaming regulations are overseen by PAGCOR.: taya777.icu – taya777.icu
Las estrategias son clave en los juegos.: jugabet.xyz – jugabet casino
https://jugabet.xyz/# Las estrategias son clave en los juegos.
Casino visits are a popular tourist attraction.
Players enjoy a variety of table games.: taya365.art – taya365
http://taya365.art/# Slot machines feature various exciting themes.
Promotions are advertised through social media channels.
taya365 login taya365 login The casino scene is constantly evolving.
Live music events often accompany gaming nights.: taya365 – taya365 com login
https://phmacao.life/# Many casinos provide shuttle services for guests.
Players must be at least 21 years old.
Las experiencias son Гєnicas en cada visita.: jugabet casino – jugabet casino
Casinos often host special holiday promotions. http://taya777.icu/# Entertainment shows are common in casinos.
http://taya777.icu/# A variety of gaming options cater to everyone.
Casinos offer delicious dining options on-site.
Slot machines feature various exciting themes.: taya777 login – taya777 app
winchile casino winchile.pro Los juegos de mesa son clГЎsicos eternos.
http://winchile.pro/# Los juegos en vivo ofrecen emociГіn adicional.
The ambiance is designed to excite players.
La seguridad es prioridad en los casinos.: jugabet chile – jugabet
Los casinos organizan eventos especiales regularmente.: jugabet casino – jugabet casino
https://taya365.art/# Players can enjoy high-stakes betting options.
Most casinos offer convenient transportation options.
Players enjoy both fun and excitement in casinos. https://winchile.pro/# Hay casinos en Santiago y ViГ±a del Mar.
https://jugabet.xyz/# Las experiencias son Гєnicas en cada visita.
A variety of gaming options cater to everyone.
La competencia entre casinos beneficia a los jugadores.: winchile casino – winchile.pro
https://phtaya.tech/# The casino scene is constantly evolving.
The Philippines offers a rich gaming culture.
phmacao com phmacao Live dealer games enhance the casino experience.
Responsible gaming initiatives are promoted actively.: taya777.icu – taya777 register login
https://phmacao.life/# Manila is home to many large casinos.
The Philippines has several world-class integrated resorts.
http://winchile.pro/# Las apuestas deportivas tambiГ©n son populares.
Players can enjoy high-stakes betting options.
taya365 login taya365 login Live dealer games enhance the casino experience.
http://jugabet.xyz/# Los croupiers son amables y profesionales.
High rollers receive exclusive treatment and bonuses.
Gambling regulations are strictly enforced in casinos.: phmacao com – phmacao
https://phtaya.tech/# The casino industry supports local economies significantly.
Most casinos offer convenient transportation options.
Live dealer games enhance the casino experience. https://winchile.pro/# La historia del juego en Chile es rica.
The casino atmosphere is thrilling and energetic.: taya777 register login – taya777 app
https://taya777.icu/# Loyalty programs reward regular customers generously.
The thrill of winning keeps players engaged.
jugabet jugabet.xyz Los bonos de bienvenida son generosos.
Players enjoy a variety of table games. https://winchile.pro/# Muchos casinos ofrecen restaurantes y bares.
Entertainment shows are common in casinos.: phmacao casino – phmacao
Los casinos celebran festivales de juego anualmente.: jugabet.xyz – jugabet casino
http://phmacao.life/# п»їCasinos in the Philippines are highly popular.
The casino scene is constantly evolving.
The gaming floors are always bustling with excitement. http://taya777.icu/# Gambling regulations are strictly enforced in casinos.
Promotions are advertised through social media channels.: phmacao – phmacao com login
https://taya365.art/# Promotions are advertised through social media channels.
The casino industry supports local economies significantly.
jugabet chile jugabet chile Los bonos de bienvenida son generosos.
https://phmacao.life/# Many casinos have beautiful ocean views.
High rollers receive exclusive treatment and bonuses.
Gambling regulations are strictly enforced in casinos. https://taya777.icu/# Many casinos host charity events and fundraisers.
Los casinos celebran festivales de juego anualmente.: jugabet – jugabet chile
Muchos casinos tienen salas de bingo.: win chile – winchile.pro
http://jugabet.xyz/# Las ganancias son una gran motivaciГіn.
Players must be at least 21 years old.
Gambling can be a social activity here. http://phmacao.life/# Gambling regulations are strictly enforced in casinos.
The Philippines has a vibrant nightlife scene.: phtaya casino – phtaya.tech
taya777 login taya777.icu Many casinos offer luxurious amenities and services.
Los bonos de bienvenida son generosos.: jugabet.xyz – jugabet casino
Gaming regulations are overseen by PAGCOR. http://jugabet.xyz/# La iluminaciГіn crea un ambiente vibrante.
La historia del juego en Chile es rica.: jugabet casino – jugabet
http://taya365.art/# Many casinos offer luxurious amenities and services.
Game rules can vary between casinos.
taya777 register login taya777 Online gaming is also growing in popularity.
http://jugabet.xyz/# Los jugadores disfrutan del pГіker en lГnea.
Many casinos have beautiful ocean views.
Entertainment shows are common in casinos. https://phmacao.life/# Casino visits are a popular tourist attraction.
Many casinos have beautiful ocean views.: taya365 – taya365
Cashless gaming options are becoming popular.: taya365 com login – taya365 login
http://winchile.pro/# Hay casinos en Santiago y ViГ±a del Mar.
The casino experience is memorable and unique.
Gambling can be a social activity here. http://phmacao.life/# The casino atmosphere is thrilling and energetic.
Muchos casinos ofrecen restaurantes y bares.: jugabet chile – jugabet casino
Manila is home to many large casinos.: phmacao – phmacao com login
http://taya365.art/# The Philippines offers a rich gaming culture.
High rollers receive exclusive treatment and bonuses.
win chile winchile casino Los casinos garantizan una experiencia de calidad.
Live music events often accompany gaming nights. http://taya777.icu/# Visitors come from around the world to play.
Los jugadores deben jugar con responsabilidad.: winchile.pro – win chile
Gambling can be a social activity here.: taya365 – taya365
http://winchile.pro/# Las apuestas deportivas tambiГ©n son populares.
Poker rooms host exciting tournaments regularly.
The casino industry supports local economies significantly. https://taya365.art/# Entertainment shows are common in casinos.
Los casinos reciben turistas de todo el mundo.: win chile – winchile
Los casinos reciben turistas de todo el mundo.: jugabet – jugabet
http://winchile.pro/# Los jugadores disfrutan del pГіker en lГnea.
Entertainment shows are common in casinos.
jugabet casino jugabet.xyz Los jackpots progresivos atraen a los jugadores.
migliori farmacie online 2024 https://farmaprodotti.com/# farmacia online senza ricetta
migliori farmacie online 2024
comprare farmaci online all’estero: farmacia online – comprare farmaci online all’estero
farmacia online
На данном сайте можно найти информацией о телешоу “Однажды в сказке”, его сюжете и главных персонажах. once upon a time сериал Здесь представлены интересные материалы о создании шоу, актерах и фактах из-за кулис.
На данном сайте вы сможете найти полезную информацию о препарате Ципралекс. Вы узнаете здесь информация о показаниях, режиме приёма и возможных побочных эффектах.
http://Lashae.omob.xyz/category/website/wgI2vZFhZf5rbhFqBTP7G0CD1
На этом сайте вы сможете найти полезную информацию о терапии депрессии у людей преклонного возраста. Вы также узнаете здесь о профилактических мерах, актуальных подходах и советах экспертов.
https://ok-vmeste.ru/toget/2487-depressija-v-starshem-vozraste-glavnye-prichiny-i-metody-lechenija.html
Стильные советы по подбору модных луков на каждый день.
Мнения экспертов, новости, все показы и мероприятия.
https://luxe-moda.ru/
Модные заметки по подбору крутых образов на любой день.
Заметки стилистов, новости, все коллекции и мероприятия.
https://metamoda.ru/moda/1141-7-prichin-lyubit-dizaynera-rick-owens/
Модные заметки по выбору отличных луков на любой день.
Заметки экспертов, события, все новинки и шоу.
https://moismi.ru/info/2024-09-15-istoriya-brenda-baldinini-ot-remeslennogo-proizvodstva-do-mezhdunarodnogo-uspeha/