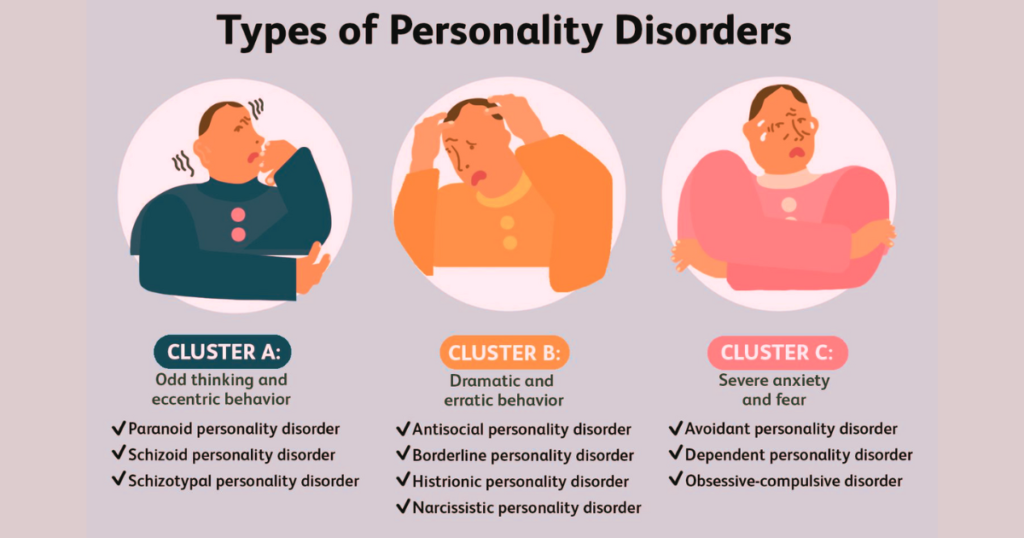
What differentiates people with obsessive-compulsive disorder (OCD) from those who don’t have OCD? OCD falls under the cluster C of personality disorders, known for their anxious and fearful behavior patterns. Obsessive-Compulsive Disorder (OCD) is a mental health condition characterized by recurring, unwanted thoughts (obsessions) and repetitive behaviors (compulsions) that a person feels driven to perform. This disorder can significantly impact daily functioning and quality of life. Here, we will explore the nature of OCD, its symptoms, causes, and treatment options, as well as practical tips for managing the condition.
What is Obsessive-Compulsive Disorder?
Obsessive-compulsive disorder is a common, chronic, and long-lasting disorder in which a person has uncontrollable, recurring thoughts (obsessions) and behaviors (compulsions) that the person feels the urge to repeat over and over. These obsessions and compulsions can be time-consuming and cause significant distress, interfering with personal, social, and professional responsibilities.
Obsessive–Compulsive Disorder Symptoms
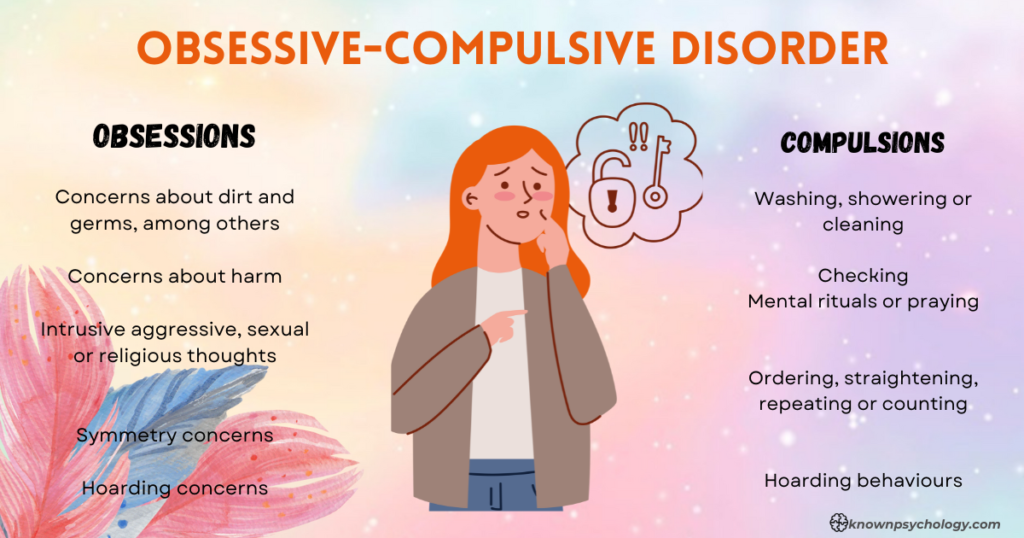
Obsessions
These are intrusive and persistent thoughts, impulses, or images that cause significant anxiety or distress. Common obsessions in OCD include:
- Contamination Fears: Fear of dirt, germs, or getting contaminated by touching objects others have touched.
- Doubting and Second-Guessing: Extreme worry about forgetting or losing something, concerns about safety or harm (e.g., fear that the stove has been left on).
- Need for Order or Symmetry: A strong need to arrange objects in a particular manner or symmetry.
- Harmful Thoughts: Fears of harming oneself or others, often through intrusive thoughts or mental images.
- Unwanted Sexual Thoughts: Unwanted sexual thoughts about inappropriate or forbidden subjects, which can include aggressive sexual behavior or fears about one’s sexual orientation.
- Religious Obsessions (Scrupulosity): Irrational religious fears, such as worrying about committing a sin or offending God.
Compulsions
These are repetitive behaviors or mental acts that a person feels driven to perform in response to an obsession, aimed at preventing or reducing distress or a feared situation. Common compulsions include:
- Washing and Cleaning: Excessive handwashing, showering, or cleaning of objects, often for much longer than necessary.
- Checking: Repeatedly checking to see if a door is locked, appliances are turned off, often performing these checks many times in a row.
- Repeating: Repeating routine activities (like going in and out of doors), body movements (like tapping or touching), or repeating sounds, words, or numbers.
- Orderliness: Arranging items to face the same way, organizing things in a specific order, or aligning objects precisely.
- Hoarding: Difficulty throwing away items regardless of actual value.
- Mental Compulsions: Mentally praying or repeating phrases to reduce anxiety, or counting while performing a task to end on a ‘good’ or ‘safe’ number.
Causes of Obsessive-Compulsive Disorder
The exact cause of OCD is not fully understood, but a combination of genetic, neurological, behavioral, cognitive, and environmental factors are believed to contribute. Some of the factors include:
- Genetics: OCD may have a component that runs in families, suggesting that genes can play a role.
- Brain Structure and Functioning: Imaging studies have shown differences in the frontal cortex and subcortical structures of the brain in those with OCD.
- Environmental Factors: Certain environmental factors such as infections are suggested to trigger OCD, but more research is needed to understand the link.
OCD Test
There isn’t a single definitive test for diagnosing Obsessive-Compulsive Disorder (OCD), but there are several methods and tools that healthcare professionals use to identify and assess the severity of OCD symptoms. The process generally involves a combination of clinical evaluation and the use of standardized assessment tools. Here are the key components of the testing and diagnosis process for OCD:
Clinical Interview
The primary method of diagnosing OCD is a detailed clinical interview conducted by a mental health professional. This may include:
- Psychiatric Assessment: Discussing symptoms, thoughts, feelings, and behavior patterns.
- Medical History: Evaluating personal and family medical history to rule out other causes of symptoms.
- Symptom Criteria Check: Using criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which requires that obsessions and compulsions must be time-consuming (taking more than one hour per day), cause significant distress, and impair social or functional abilities.
Self-Report Questionnaires
Several standardized questionnaires can help identify OCD symptoms and gauge their severity. These include:
- Yale-Brown Obsessive Compulsive Scale (Y-BOCS): A widely used scale that measures the severity of obsessions and compulsions.
- Obsessive-Compulsive Inventory (OCI): A self-rated scale that covers different symptoms of OCD and assesses their severity.
- Padua Inventory: Another inventory that assesses the severity of a wide range of OCD symptoms.
Psychological Evaluation
Further psychological testing might be done to evaluate cognitive functions and emotional states, helping to distinguish OCD from other conditions like anxiety disorders or depression.
Physical Examination
Although not used to diagnose OCD directly, a physical examination might be conducted to rule out other medical conditions that could be causing the symptoms.
Monitoring and Follow-Up
Since OCD often coexists with other disorders, ongoing assessment and monitoring are crucial. This can help in adjusting treatment plans as needed and addressing any additional mental health issues.
Importance of Professional Diagnosis
It’s important for anyone who suspects they might have OCD to seek a formal diagnosis from a qualified mental health professional. Self-diagnosis or using online tests can lead to inaccuracies and should not replace professional evaluation.
Getting diagnosed by a professional is crucial, as they can provide the right treatment options such as cognitive-behavioral therapy (CBT), medications, or a combination, which have been proven effective for many people with OCD.
Obsessive-Compulsive Disorder Treatment
Treatment for Obsessive-Compulsive Disorder (OCD) is generally focused on two main approaches: psychological therapy and medications. These treatments can be highly effective, reducing the symptoms or even bringing the disorder into remission. The best approach often depends on the severity of the condition, the individual’s preferences, and their overall health. Here’s a breakdown of the primary treatment options for OCD:
1. Psychological Therapy
Cognitive Behavioral Therapy (CBT) is considered the most effective form of psychological treatment for OCD. Within CBT, a specific technique called Exposure and Response Prevention (ERP) is especially beneficial:
- Exposure and Response Prevention (ERP): This involves exposing the person to situations and objects that trigger their OCD compulsions, and then helping them learn to refrain from performing the compulsive behavior. Over time, ERP can significantly reduce OCD symptoms by teaching the patient to tolerate the anxiety associated with the obsessions without performing compulsive acts.
- Other forms of CBT: These might focus on challenging and changing the unhelpful beliefs related to the obsessions (cognitive therapy), improving stress management, and enhancing overall emotional regulation.
2. Medications
Certain medications, particularly those that affect the neurotransmitter serotonin, are useful in treating OCD. These include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): These are typically the first choice in medication treatment for OCD. Examples include fluoxetine (Prozac), fluvoxamine (Luvox), sertraline (Zoloft), and paroxetine (Paxil). It may take several weeks to see improvements, and treatment is often continued for one to two years, or even longer in some cases.
- Tricyclic Antidepressants (TCAs): In cases where SSRIs are not effective, tricyclic antidepressants like clomipramine (Anafranil) might be used. Clomipramine is known for being particularly effective in treating OCD but often has more side effects than SSRIs.
3. Advanced Treatments
For severe cases of OCD that do not respond to the usual treatments, more advanced options may be considered:
- Deep Brain Stimulation (DBS): This involves implanting electrodes in specific areas of the brain and is approved under certain circumstances for severe cases of OCD.
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain.
- Residential Treatment Programs: These provide intensive and structured treatment for severe OCD and are an option when outpatient treatments have been unsuccessful.
4. Lifestyle and Home Remedies
In addition to formal treatment, certain lifestyle adjustments can help manage symptoms:
- Stress Management Techniques: Regular exercise, meditation, and mindfulness can reduce the overall anxiety and stress that may exacerbate OCD symptoms.
- Support Groups: Joining OCD support groups where experiences and coping strategies are shared can be very beneficial.
5. Integrated Treatment Plans
An integrated approach that combines medication, therapy, and lifestyle changes typically offers the best outcomes. Regular follow-up with mental health professionals ensures that the treatment plan remains effective and can be adjusted as needed.
Effective treatment for OCD requires a tailored approach, consistent follow-up, and sometimes trying different treatments to manage the disorder effectively.
A note from Known_Psychchology
OCD is a challenging disorder, but with effective treatment and management strategies, individuals can regain control over their lives. If you or someone you know is struggling with OCD, it is crucial to seek professional help. With the right support, individuals with OCD can lead a fulfilling life, managing their symptoms effectively.
References
- American Psychiatric Association. 2022. What Is Obsessive-Compulsive Disorder?
- Brock H, Hany M. 2022. Obsessive-Compulsive Disorder. https://www.ncbi.nlm.nih.gov/books/NBK553162/.
- International OCD Foundation. What is OCD? https://iocdf.org/about-ocd/.
- Merck Manual: Professional Version. Obsessive-Compulsive Disorder (OCD). https://www.merckmanuals.com/professional/psychiatric-disorders/obsessive-compulsive-and-related-disorders/obsessive-compulsive-disorder-ocd.
- National Institute of Mental Health. Obsessive-Compulsive Disorder.

Pingback: What I learned from a week of contemplating my death – Hard in Scientific
Pingback: Understanding Obsessive Compulsive Disorder and Treatment
Pingback: Understanding Obsessive Compulsive Disorder and Treatment - BlogBursts 100% Free Guest Posting Website