The relationship between mental health disorders and addiction is complex and often intertwined. Understanding co-occurring disorders is vital in today’s society, where many individuals face the dual challenge of managing both mental health and addiction issues.
Understanding Co-Occurring Disorders
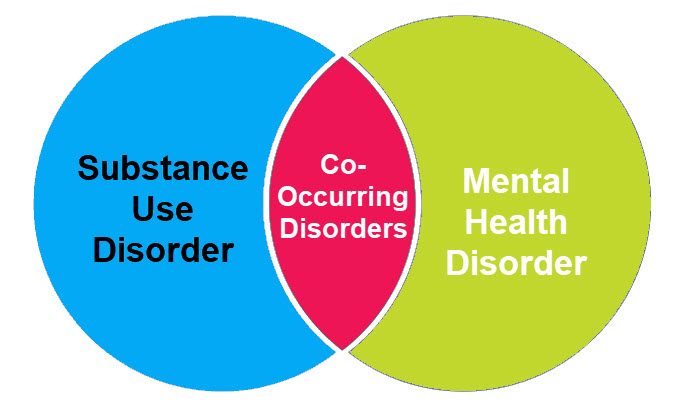
The relationship between mental health and addiction is complex and deeply intertwined. Co-occurring disorders, also known as dual diagnoses, refer to the simultaneous presence of a mental health condition and a substance use disorder. This connection is not uncommon, as individuals often turn to drugs or alcohol to cope with the symptoms of mental health challenges like depression, anxiety, PTSD, or bipolar disorder. Unfortunately, substance use can exacerbate these symptoms, creating a vicious cycle that is difficult to break.
Mental health disorders can alter brain chemistry, making individuals more vulnerable to the addictive properties of substances. Conversely, chronic substance use can contribute to the development of mental health conditions by disrupting emotional regulation and increasing feelings of hopelessness or isolation.
Effective treatment for co-occurring disorders requires an integrated approach that addresses both conditions simultaneously. This may involve a combination of therapies such as cognitive-behavioral therapy (CBT), medication management, and support groups. It’s also important to focus on building healthy coping mechanisms and fostering a strong support system.
Understanding the mental health-addiction connection is key to breaking the stigma and encouraging individuals to seek help. With the right treatment and support, recovery from co-occurring disorders is not only possible but sustainable.
The Staggering Statistics of Co-occurring Disorders
Recent research indicates that approximately 9 million adults in the United States experience co-occurring disorders. This staggering statistic highlights a pressing issue that demands attention and action.
The Complex Interplay: Why Mental Health and Addiction Often Coexist
Mental health disorders and addiction often feed into one another, creating a vicious cycle. When individuals suffer from mental health issues, they may turn to drugs or alcohol to cope. Conversely, addiction can exacerbate mental health conditions, making recovery more difficult. This “chicken-or-egg” phenomenon complicates understanding and treatment.
The Importance of Understanding This Connection for Effective Treatment
Recognizing the link between mental health disorders and addiction is crucial for effective treatment. Holistic approaches that address both conditions simultaneously stand a better chance at fostering recovery.
Understanding Mental Health Disorders
Common Mental Health Disorders that Co-occur with Addiction
Several mental health disorders show a high rate of co-occurrence with addiction, including:
- Depression: Associated with feelings of sadness and hopelessness. Studies show that about 30% of individuals with depression also have a substance use disorder.
- Anxiety Disorders: Includes generalized anxiety, panic disorder, and social anxiety. Approximately 20% of individuals with anxiety disorders turn to substances for relief.
- Bipolar Disorder: Characterized by extreme mood swings. Roughly 56% of people with bipolar disorder also struggle with addiction.
- Post-Traumatic Stress Disorder (PTSD): Often seen in individuals who have experienced trauma. Around 33% of people with PTSD have substance use problems.
The Symptoms and Impact of These Disorders
Common symptoms of mental health disorders include:
- Persistent sadness
- Mood swings
- Excessive worry
- Flashbacks or intrusive thoughts
These symptoms significantly impact one’s daily life, affecting relationships, job performance, and general well-being.
Seeking Professional Diagnosis and Treatment
Consulting a mental health professional is critical for accurate diagnosis and tailored treatment options. Early intervention can lead to better outcomes.
Understanding Addiction
Defining Addiction: Beyond Substance Abuse
Addiction can involve more than just substance abuse. It also includes behavioral addictions, such as gambling or internet addiction. Both types can lead to negative consequences in life.
The Role of Neurobiology in Addiction
Addiction alters brain chemistry, affecting areas responsible for pleasure, impulse control, and decision-making. Understanding these neurobiological factors is key to appreciating the challenges of recovery.
Common Substances and Behaviors Involved in Addiction
Common substances include:
- Alcohol
- Opioids
- Cocaine
- Nicotine
Behavioral addictions may involve activities like gambling, gaming, or compulsive shopping. Each of these can have detrimental effects on mental health.
The Intertwined Relationship: How They Influence Each Other
The Self-Medication Hypothesis
Many people with mental health disorders may use substances as a form of self-medication. This approach provides temporary relief but ultimately leads to worse outcomes.
The Shared Risk Factors
Several overlapping risk factors contribute to both addiction and mental illness:
- Genetics: Family history can predispose individuals to both conditions.
- Trauma: Experiencing traumatic events increases the likelihood of developing both issues.
- Stress: High-stress environments can trigger both mental health issues and substance use.
The Cycle of Co-occurring Disorders
The interplay between mental health and addiction can create a cycle that is hard to break. One serves to worsen the other, making recovery a challenging journey.
Effective Treatment Approaches for Co-occurring Disorders
Integrated Treatment Models: The Importance of Holistic Care
Integrated treatment models combine strategies for treating both mental health disorders and addiction. This holistic approach improves recovery chances and overall well-being.
Therapy Options for Co-occurring Disorders
Several therapy types are effective for managing both conditions, including:
- Cognitive Behavioral Therapy (CBT)
- Dialectical Behavior Therapy (DBT)
- Group Therapy
These modalities provide support and tools for coping with both mental health and addiction issues.
Medication Management in Co-occurring Disorders
In some cases, medications may be necessary to manage mental health symptoms. A healthcare professional can guide the best options while considering potential interactions with substances.
Seeking Help and Support
Recognizing the Signs of Co-occurring Disorders
Common warning signs include:
- Increased substance use
- Changes in mood or behavior
- Difficulty maintaining relationships
- Neglecting responsibilities
Identifying these signs early can lead to timely intervention.
Finding the Right Treatment Provider
Locating a treatment provider specializing in co-occurring disorders involves research. Look for licensed professionals who understand both addiction and mental health.
Support Networks and Resources for Recovery
Numerous resources exist for those on the recovery journey:
- National Alliance on Mental Illness (NAMI)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Local support groups
These networks provide information and support for individuals and families.
Conclusion
Key Takeaways: Understanding and Addressing Co-occurring Disorders
Understanding the connection between mental health disorders and addiction is a vital step toward recovery. Knowledge of symptoms, risk factors, and addiction treatment options empowers individuals to seek help.
A Path Towards Recovery and Well-being
Hope exists for those struggling with co-occurring disorders. Recovery is a path paved with support, knowledge, and professional guidance. Seek help to reclaim your well-being and live a fulfilling life.
Mariam holds an MS in Sociology with a specialization in Medical Sociology and Social Psychology. With a strong academic background and extensive research work in both fields, she brings depth and clarity to complex topics. Her writing explores the intersection of society, health, and the human mind, making academic ideas easy to grasp and relevant to everyday life.


