Schizotypal Personality Disorder (SPD) occupies a unique place in the landscape of mental health, nestled within the spectrum of personality disorders yet distinct in its characteristics and impact on individuals. It is a condition marked by pervasive patterns of social and interpersonal deficits, along with acute discomfort in close relationships, cognitive or perceptual distortions, and eccentricities in behavior. Understanding SPD is not just about identifying symptoms—it’s about empathizing with the experiences of those who live with it, recognizing the challenges they face, and exploring the pathways to support and treatment.
This blog aims to shed light on the nuances of Schizotypal Personality Disorder, providing insights into its symptoms, causes, and the hope that therapy and understanding can bring to those affected.
What is Schizotypal Personality Disorder?
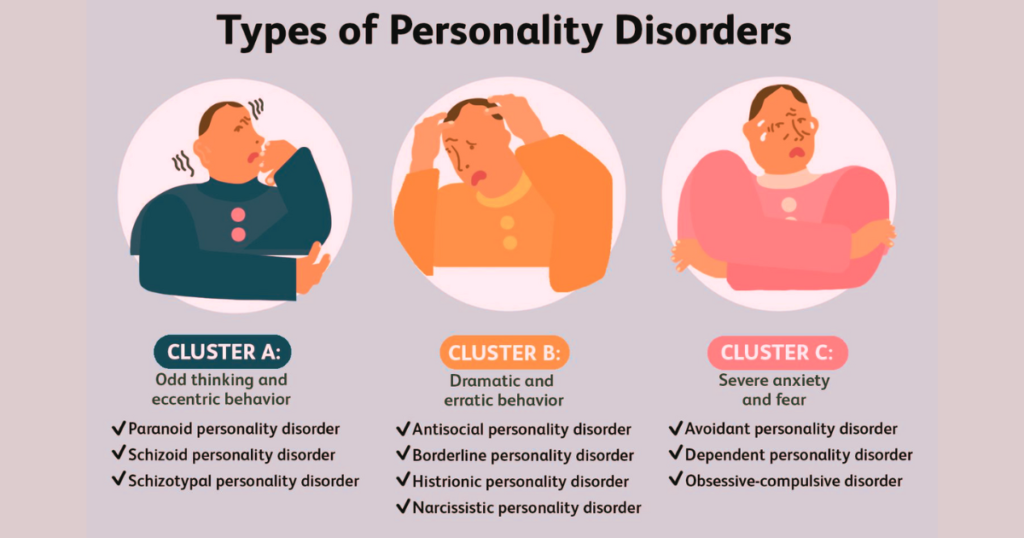
Schizotypal Personality Disorder (SPD) is a mental health condition characterized by significant discomfort in close relationships, distorted thinking, and eccentric behavior. Individuals with SPD often experience acute discomfort with, and reduced capacity for, close relationships. They typically display a pattern of peculiarities in their thinking, behavior, and appearance, such as having odd beliefs or magical thinking that influences behavior and is inconsistent with subcultural norms. These individuals may also exhibit unusual perceptual experiences, including bodily illusions or odd speech patterns, which can make their communication seem vague or disjointed. While they may desire close relationships, their social anxiety, paranoia, and odd behaviors often alienate others, leading to a pattern of social and interpersonal deficits.
Schizotypal Personality Disorder is distinct from schizophrenia and other personality disorders, though it falls within the schizophrenia spectrum disorders due to shared symptoms and genetic risk factors. Unlike schizophrenia, which is characterized by more severe symptoms such as delusions, hallucinations, and a significant loss of contact with reality, SPD symptoms are less intense and do not include the full-blown psychotic symptoms seen in schizophrenia. Individuals with SPD maintain a grasp on reality, although they may experience transient psychotic episodes, especially under stress.
Compared to other personality disorders, SPD is unique in its emphasis on peculiar thought patterns, perceptions, and behaviors. While there may be overlaps, such as with schizoid personality disorder (characterized by social detachment and restricted emotional expression), the eccentricities and distorted cognitions of SPD set it apart.
Symptoms of Schizotypal Personality Disorder
Schizotypal Personality Disorder (SPD) manifests through a range of symptoms that significantly affect interpersonal relationships and daily functioning. These symptoms are often noticeable in late adolescence or early adulthood and can impact various aspects of life. Here’s a detailed look at the key symptoms associated with SPD:
- Peculiar Behavior or Appearance: Individuals with SPD may have an eccentric appearance, exhibiting unusual clothing or grooming habits that don’t align with cultural norms. Their behaviors can also be perceived as odd or unconventional.
- Social Anxiety and Discomfort: Despite a desire for social interaction, people with SPD experience intense discomfort in social situations, often due to a deep-seated fear of negative evaluation or rejection. This anxiety tends to persist and does not diminish with familiarity, distinguishing it from more generalized social anxieties.
- Odd Beliefs or Magical Thinking: Those with SPD may believe in telepathy, clairvoyance, or other forms of extrasensory perception. They might also have superstitions or preoccupations with paranormal phenomena that influence their behavior and are inconsistent with cultural norms.
- Unusual Perceptual Experiences: Individuals may report perceptual alterations that could include feeling the presence of a force or person not actually present, hearing a voice whispering their name, or other sensory distortions that are not full-blown hallucinations.
- Odd or Paranoid Thoughts and Speech Patterns: Speech may be unusual without being incoherent; it can include vague, circumstantial, metaphorical, or overly elaborate patterns of speech. Paranoid thoughts and suspiciousness about others’ motivations are common.
- Emotional Detachment or Inappropriateness: There can be a noticeable lack of response to social cues, leading to inappropriate emotional reactions or a flat affect. Emotional expression may be limited, and there can be a significant detachment from social relationships.
- Lack of Close Friends or Confidants: Except for family members, individuals with SPD often have a very limited circle of intimate relationships. Their discomfort with social interaction and odd behaviors can make forming close friendships challenging.
- Excessive Social Anxiety: Unlike typical social anxiety, which might lessen as individuals become more familiar with others, the anxiety experienced by people with SPD is often linked to paranoid fears rather than judgments about self-worth.
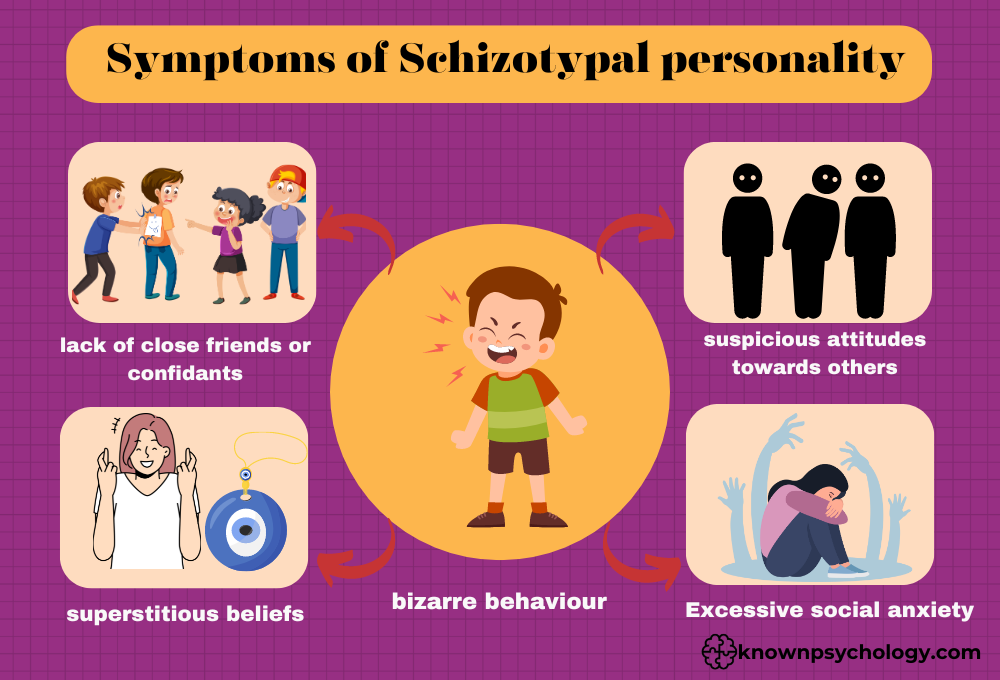
These symptoms can vary in intensity and may fluctuate over time. It’s important to note that not everyone with SPD will experience all these symptoms, and the presence of several of these characteristics can significantly impact an individual’s quality of life, requiring professional support and intervention.
Causes and Risk Factors
The causes and risk factors of Schizotypal Personality Disorder (SPD) are multifaceted, involving a complex interplay of genetic, neurobiological, and environmental factors. Understanding these factors can help in identifying potential risks and early intervention strategies.
Genetic and Familial Factors:
- Genetic Predisposition: There’s a significant genetic component to SPD, with research indicating that it is more common in individuals who have family members with schizophrenia or other schizophrenia spectrum disorders. This suggests a hereditary risk, with certain genes possibly increasing susceptibility to the disorder.
- Family History: A family history of any personality disorders or mental health conditions can increase the risk of developing SPD. The exact genetic markers and the mechanism of inheritance remain areas of ongoing research.
Neurobiological Factors:
- Brain Structure and Function: Neuroimaging studies have shown differences in the brain structures and functions of individuals with SPD compared to those without the disorder. These differences often involve areas associated with emotion regulation, social cognition, and sensory processing. However, the relationship between these neurobiological differences and SPD symptoms is not fully understood.
- Neurotransmitter Imbalances: Abnormalities in neurotransmitter systems, particularly dopamine, may play a role in the development of SPD. Dopamine is involved in the regulation of mood, perception, and thought processes, and imbalances can contribute to the symptomatology of SPD.
Environmental Factors:
- Early Life Experiences: Early childhood experiences, including trauma, neglect, or a lack of stable relationships, can increase the risk of developing SPD. These experiences can affect personality development and the ability to form healthy relationships.
- Social Isolation: Persistent social isolation, whether voluntary or involuntary, can exacerbate or contribute to the development of schizotypal traits. Lack of social interaction during critical developmental periods can impair social and emotional development.
- Parenting Styles: Certain parenting styles, particularly those that are overly controlling or emotionally detached, have been suggested as potential risk factors for the development of personality disorders, including SPD.
Psychosocial Factors:
- Stress and Coping Mechanisms: High levels of stress and inadequate coping mechanisms can trigger or worsen the symptoms of SPD. Individuals with SPD may have a lower threshold for stress, and their peculiar behaviors and thought patterns can be, in part, coping mechanisms for stress and anxiety.
- Cultural and Societal Influences: Cultural and societal factors can influence the expression of SPD symptoms and the likelihood of seeking treatment. In some cultures, behaviors and beliefs associated with SPD may be more accepted or interpreted differently, affecting diagnosis and management.
It’s important to note that having one or more of these risk factors does not guarantee that a person will develop SPD. The disorder likely results from a combination of these factors rather than any single cause. Further research is needed to fully understand the etiology of SPD and to develop targeted prevention and intervention strategies.
Impact of Schizotypal Personality Disorder(SPD) on Daily Life
Schizotypal Personality Disorder (SPD) significantly impacts various aspects of daily life and functioning for those affected by it. The peculiar behaviors, distorted thinking, and social anxiety associated with SPD can lead to comprehensive challenges in personal, social, and professional domains.
Personal and Social Life:
Individuals with SPD often struggle with forming and maintaining close relationships. Their acute discomfort in social situations, coupled with eccentric behaviors and odd speech, can make social interactions daunting and confusing for both the individual and others. This may result in a pattern of isolation and a profound sense of loneliness. Their unusual beliefs and perceptions can also make it difficult for them to relate to others, leading to misunderstandings and strained relationships. The social anxiety and paranoia that often accompany SPD can exacerbate these issues, making individuals reluctant to engage in social activities or form new friendships.
Professional Life and Employment:
The symptoms of SPD can also create barriers to professional success and satisfaction. The disorder’s impact on communication skills and social interaction can make teamwork and workplace relationships challenging. Individuals may struggle to fit into organizational cultures or to adhere to social norms at work, potentially leading to job instability or dissatisfaction. Their unique way of thinking and perceiving the world, while potentially beneficial in creative roles, may also be misunderstood or undervalued in more conventional work environments.
Education:
The challenges of SPD extend to educational settings as well. Students with SPD may find it difficult to participate in group activities or to engage with peers and instructors. Their social anxiety and eccentric behavior can hinder academic performance and participation. Furthermore, the disorder can affect their ability to concentrate and process information, potentially impacting learning and academic success.
Self-Care and Independence:
Daily living and self-care can also be affected by SPD. The lack of close relationships may mean individuals have less support when dealing with life’s challenges. Their struggle with initiating and organizing tasks, stemming from their symptoms, can make managing daily responsibilities and self-care difficult. This can lead to a reliance on family members or social services for assistance with basic needs and healthcare.
Emotional Health:
Beyond the social and practical aspects of life, SPD impacts emotional well-being. The constant sense of being different, along with difficulties in expressing emotions and experiencing close relationships, can lead to feelings of alienation, depression, and low self-esteem. The stress of attempting to navigate a world that feels bewildering and sometimes hostile can exacerbate these feelings.
Overall, the impact of Schizotypal Personality Disorder on daily life is profound and pervasive. However, with appropriate treatment and support, individuals with SPD can learn coping strategies to manage their symptoms, improve social skills, and lead fulfilling lives. Therapy, social skills training, and sometimes medication can help manage the symptoms of SPD, enabling individuals to navigate their daily lives more effectively.
Diagnosis and Treatment of Schizotypal Personality Disorder (SPD)
Diagnostic Criteria and Process
The diagnostic criteria for Schizotypal Personality Disorder, as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM), include a range of symptoms related to social and interpersonal deficits, cognitive or perceptual distortions, and eccentricities in behavior. To be diagnosed with SPD, individuals must exhibit a pervasive pattern of social and interpersonal limitations marked by acute discomfort in close relationships, cognitive or perceptual distortions, and eccentric behavior.
This includes symptoms such as ideas of reference (excluding delusions of reference), odd beliefs or magical thinking, unusual perceptual experiences, odd thinking and speech, suspiciousness or paranoid ideation, inappropriate or constricted affect, behavior or appearance that is odd, eccentric, or peculiar, lack of close friends or confidants outside of first-degree relatives, and excessive social anxiety that does not diminish with familiarity.
The diagnostic process typically involves a comprehensive psychiatric evaluation, including a thorough medical history, and may use structured psychological interviews and questionnaires. Diagnosis is often complex, requiring differentiation from other mental health disorders, such as schizophrenia, schizoid personality disorder, and bipolar disorder, among others. It’s essential that the evaluation is conducted by a mental health professional trained in diagnosing personality disorders.
Psychotherapy Approaches
Cognitive Behavioral Therapy (CBT): CBT is often effective for treating SPD. It helps individuals identify and challenge distorted patterns of thinking and behavior, aiming to reduce social anxiety, improve social skills, and address any co-occurring conditions, such as depression. CBT can also help in managing paranoia and reducing the severity of disordered thinking.
Dialectical Behavior Therapy (DBT): Originally developed for borderline personality disorder, DBT has been adapted for SPD to help individuals manage emotions, develop stress tolerance skills, and improve interpersonal effectiveness. DBT focuses on mindfulness and acceptance strategies, which can be particularly helpful for those with SPD in managing their symptoms.
Medication Management
While there are no medications specifically approved for the treatment of SPD, medications may be prescribed to address specific symptoms or co-occurring conditions. Antipsychotic medications may be used to help manage acute psychotic symptoms, if present. Antidepressants may be prescribed for depressive symptoms, and anxiolytics may be used to reduce social anxiety. The use of medication is typically considered adjunctive to psychotherapy and tailored to the individual’s specific symptom profile.
Importance of a Supportive Therapeutic Relationship
A supportive therapeutic relationship is crucial in the treatment of SPD. Individuals with SPD often have significant trust issues and may be suspicious of the therapist’s intentions. Building a strong therapeutic alliance can help overcome these barriers. A therapist who is empathetic, patient, and consistent can provide a safe space for the individual to explore their thoughts, behaviors, and emotions. This supportive relationship is foundational to engaging the individual in therapy, encouraging them to stay in treatment, and facilitating their progress toward healthier functioning.
Effective treatment of SPD requires a comprehensive, individualized approach that considers the unique challenges and strengths of each person. With appropriate intervention, individuals with SPD can achieve improved social functioning and quality of life.
Strategies for Managing Symptoms
Managing symptoms of Schizotypal Personality Disorder (SPD) involves a multifaceted approach that combines professional mental health support with self-care practices. Here are detailed strategies for managing symptoms:
- Professional Therapy: As discussed above engaging in therapies such as Cognitive Behavioral Therapy (CBT) can help individuals understand and change distorted thought patterns and behaviors. Psychotherapy can also focus on improving social skills and reducing social anxiety, which are core challenges for those with SPD.
- Medication: While there’s no specific medication for SPD, doctors may prescribe medications to address specific symptoms, such as antidepressants for depression or antipsychotics for severe symptoms like transient psychosis. It’s crucial to have a thorough evaluation and ongoing monitoring by a healthcare provider.
- Building Social Skills: Gradual exposure to social situations and structured social skills training can help individuals with SPD develop better interpersonal communication. This might include role-playing, social cues education, or participation in therapy groups.
- Stress Management: Because stress can exacerbate symptoms, learning stress reduction techniques such as mindfulness, meditation, and deep breathing exercises can be beneficial.
- Routine and Structure: Establishing a daily routine can provide a sense of structure and predictability, reducing stress and helping manage day-to-day challenges.
- Creative Expression: Engaging in creative activities like art, music, or writing can offer an outlet for expressing thoughts and emotions in a constructive and therapeutic way.
- Healthy Lifestyle Choices: Regular physical activity, a balanced diet, and adequate sleep can have a significant positive impact on mental health and help mitigate some symptoms of SPD.
The Role of Support Networks and Communities
The role of support networks and communities in managing Schizotypal Personality Disorder cannot be overstated. Here’s how they contribute:
- Emotional Support: Having a support network provides individuals with a sense of belonging and acceptance. Emotional support from family, friends, or support groups can offer comfort and reduce feelings of isolation.
- Understanding and Acceptance: Communities and support networks familiar with SPD can offer a non-judgmental space for individuals to share their experiences and challenges. This understanding environment fosters acceptance and empathy, crucial for emotional well-being.
- Resource Sharing: Support groups and communities often share resources about managing SPD, including coping strategies, recommendations for therapists or treatments, and educational materials. This information can be invaluable for someone navigating the complexities of the disorder.
- Motivation and Encouragement: Support from others can motivate individuals with SPD to adhere to their treatment plans, engage in social activities, and practice self-care strategies. Encouragement from peers who have faced similar challenges can inspire hope and perseverance.
- Social Skills Practice: Support groups or community gatherings can provide a safe environment for individuals with SPD to practice social skills and interactions, reducing social anxiety and improving confidence in social settings.
Engagement in therapy, combined with a supportive community and healthy lifestyle choices, forms a comprehensive approach to managing Schizotypal Personality Disorder. These strategies emphasize the importance of professional guidance while recognizing the value of support and personal agency in navigating SPD.
Sum up
In conclusion, managing Schizotypal Personality Disorder requires a holistic and individualized approach that combines professional treatment, self-care, and the unwavering support of communities and networks. Through a combination of therapy, possibly medication, skill development, and lifestyle adjustments, individuals with SPD can navigate the complexities of their symptoms with greater resilience. Support networks play a pivotal role in providing emotional sustenance, understanding, and practical assistance, helping to reduce isolation and foster a sense of belonging. By embracing these strategies and leveraging the strength of community connections, those affected by SPD can work towards leading more fulfilling lives, characterized by improved social interactions and a better understanding of themselves and their unique perspectives.
Known Psychology is a collaborative platform run by a dedicated team of psychology experts, professional writers, and experienced editors who are passionate about psychology and mental wellness. We publish evidence-based, easy-to-understand content designed to inform, inspire, and support our global audience. Every article is carefully researched and crafted to provide reliable insights into human behavior, emotional health, therapy techniques, and personal growth strategies. At Known Psychology, we turn complex psychological topics into simple, actionable knowledge.

I was able to find good information from your content.
Hello I absolutely love your article and it has been so admirable hence I am going to save it. I Have to say the Superb research you have done is greatly
Way cool! Some extremely valid points! I appreciate you penning this write-up and the rest of the website is really good.
In show date leading to a net insurance policies, agencies, providers and in addition all the other businesses, were actually limited in your methods make could definitely advertise themselves with the aid of television, tabloids, radio or anything else.
As usual you did an great job evaluating the problem and finding a good answer. I will stay tuned for more releases on your blog.
That is a great tip particularly to those fresh to the blogosphere. Short but very accurate info… Thank you for sharing this one. A must read post.
Great article! I learned a lot from your detailed explanation. Looking forward to more informative content like this!
Spot on with this write-up, I absolutely believe this website needs far more attention. I’ll probably be back again to see more, thanks for the advice!
Excellent post! We are linking to this great article on our site. Keep up the good writing.
If you really want you can look the other way and not talk about it. The best thing you can do is become relevant with yourself and faithful with your own morals. Generally this will lead to a mistaken and unproductive life.
Appreciating the persistence you’d put in to the blog – Gulvafslibning | Kurt Gulvmand as well as in depth information you present… It’s good to come upon a different blog once in a while that is not similar unwanted re-written material. Great read. I’ve bookmarked your blog post and I’m adding your Rss feeds to my Bing address … FYI what about Egypt wonderful tv news…
A person essentially help to make seriously articles I would state. This is the first time I frequented your web page and thus far? I surprised with the research you made to create this particular publish amazing. Great job!
This was a great read! Your insights are truly helpful and make complex topics easy to understand. Looking forward to more!
This blog was… how do I say it? Relevant!! Finally I’ve found something which helped me. Cheers.
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
I am typically to blogging and i actually appreciate your content regularly. Your content has truly peaks my interest. I am going to bookmark your web site and maintain checking for new info.
There is noticeably a lot to know about this. I believe you made some nice points in features also.
Along with every little thing that appears to be building within this particular area, many of your opinions are generally fairly radical. Nevertheless, I am sorry, but I do not subscribe to your whole strategy, all be it radical none the less. It looks to everyone that your remarks are generally not completely rationalized and in simple fact you are your self not even entirely convinced of the argument. In any case I did enjoy looking at it.
This was a great read! Your insights are truly helpful and make complex topics easy to understand. Looking forward to more!
It is one of the world’s oldest gemstones.
All you need to know about African Mangoo fully explained.
Aw, this became an exceptionally nice post. In idea I have to set up writing like this additionally – taking time and actual effort to make a good article… but so what can I say… I procrastinate alot and also by no means manage to go accomplished.
pay per click programs are really great, i could earn some decent cash from it-
Well-written and insightful! Your points are spot on, and I found the information very useful. Keep up the great work!
Good post. I learn something totally new and challenging on blogs I stumbleupon on a daily basis. It’s always exciting to read articles from other authors and use a little something from their websites.
Just determined your blog site a week ago and i also may be perusing they always. There’s a a lot of information next and i really enjoy your thing through the web presence additionally. Preserve the nice employment!
Along with the budget and special effects, or to be more accurate, more importantly then the technical elements, Star Trek pulsates with life and the human element thanks to a superb ensemble cast.
It¡¦s actually a great and useful piece of information. I am happy that you shared this helpful information with us. Please keep us informed like this. Thanks for sharing.
Well-written and insightful! Your points are spot on, and I found the information very useful. Keep up the great work!
Lenders make selections concerning the creditworthiness of borrowers primarily based primarily on credit studies and credit scores — two methods to quickly assess an applicant’s credit history.
Fantastic post! The information you shared is really valuable and well-explained. Thanks for putting this together!
After I initially left a comment I seem to have clicked the -Notify me when new comments are added- checkbox and now each time a comment is added I get 4 emails with the exact same comment. Is there a way you can remove me from that service? Appreciate it.
Introducing to you the most prestigious online entertainment address today. Visit now to experience now!
Next time I read a blog, Hopefully it doesn’t disappoint me just as much as this one. After all, I know it was my choice to read through, nonetheless I actually thought you’d have something useful to talk about. All I hear is a bunch of moaning about something that you could possibly fix if you were not too busy searching for attention.
I was able to find good advice from your articles.
I want to to thank you for this very good read!! I absolutely loved every bit of it. I’ve got you bookmarked to look at new things you post…
Fantastic post! The information you shared is really valuable and well-explained. Thanks for putting this together!
I adore your wp theme, wherever do you down load it from?
Sweet blog! I found it while browsing on Yahoo News. Do you have any tips on how to get listed in Yahoo News? I’ve been trying for a while but I never seem to get there! Thanks
Hi, just wanted you to know I have added your site to my Google bookmarks because of your special blog layout. But earnestly, I think your site has one of the cleverest theme I’ve came across. It really helps make reading your blog a lot better.
Greetings! Very helpful advice in this particular article! It’s the little changes that will make the greatest changes. Thanks a lot for sharing!
I truly love your website.. Pleasant colors & theme. Did you build this web site yourself? Please reply back as I’m wanting to create my very own website and want to find out where you got this from or exactly what the theme is named. Thank you!
Fantastic post! The information you shared is really valuable and well-explained. Thanks for putting this together!
Excellent article! We will be linking to this great post on our website. Keep up the good writing.
Having read this I thought it was rather informative. I appreciate you taking the time and energy to put this content together. I once again find myself spending a significant amount of time both reading and leaving comments. But so what, it was still worth it.
Bpi net empresas Portugal, bpi net empresas Serviços. Plataforma de comunicação Multibancária · Canal SWIFT Net · App BPI Empresas · BPI Net Empresas. Tudo Sobre. Open Banking · Segurança Online
Navies of the Second World Battle.
Everything is very open with a precise description of the issues. It was definitely informative. Your site is extremely helpful. Thank you for sharing!
Spot on with this write-up, I seriously feel this website needs much more attention. I’ll probably be back again to read through more, thanks for the information!
I start to hate this junk e-mail from writing here figures on the forums… Your journal looks as unoccupied without… Would You like to serve me and show to all the know-how you are using if You’re fighting against the spamers? TX
A hyper-efficient decentralized crypto marketplace built on Sui. Turbos finance Trade Trade any crypto on Sui. Best prices are offered through aggregating liquidity.
I have to express some appreciation to the writer just for rescuing me from this type of dilemma. Just after looking out through the search engines and obtaining techniques that were not pleasant, I believed my life was over. Existing without the presence of answers to the issues you’ve sorted out through your entire guideline is a crucial case, as well as those which could have in a wrong way damaged my career if I hadn’t come across the website. The talents and kindness in touching all the details was very helpful. I don’t know what I would have done if I had not encountered such a point like this. I can at this point look ahead to my future. Thank you very much for the high quality and results-oriented help. I won’t be reluctant to recommend your site to anyone who needs guidelines about this matter.
I’ve been exploring for a little for any high-quality articles or weblog posts on this kind of area . Exploring in Yahoo I finally stumbled upon this web site. Reading this information So i’m glad to express that I’ve an incredibly good uncanny feeling I discovered just what I needed. I most no doubt will make sure to don’t forget this website and give it a glance regularly.
Balances Active Orders Withdraw Deposit TradeOgre Logout · Sign In. Search: Currency, Market, Change, Price
A hyper-efficient decentralized crypto marketplace built on Sui. Turbos finance Sui Trade Trade any crypto on Sui. Best prices are offered through aggregating liquidity.
With furnishings, window remedies, and artwork banished, the room’s pluses — and minuses — are exposed.
You actually make it seem so easy with your presentation but I find this topic to be really something that I think I would never understand. It seems too complicated and very broad for me. I’m looking forward for your next post, I’ll try to get the hang of it!
I think your blog is very popular on this topic judging by all the other comments posted to it
the baby cribs should be as protected as possible and it should have additiona safety features..
I really enjoyed reading this! Your writing style is engaging, and the content is valuable. Excited to see more from you!
Nice post. I learn something new and challenging on sites I stumbleupon on a daily basis. It will always be helpful to read articles from other authors and practice a little something from other websites.
Sweet website , super layout, really clean and utilize genial .
you have a very wonderful weblog here! do you want to cook some invite posts on my weblog?
Thanks for sharing your ideas with this blog. Likewise, a misconception regarding the financial institutions intentions while talking about foreclosure is that the financial institution will not getreceive my repayments. There is a certain amount of time in which the bank will require payments here and there. If you are as well deep inside the hole, they may commonly desire that you pay the actual payment in full. However, i am not saying that they will have any sort of repayments at all. When you and the loan company can have the ability to work anything out, your foreclosure process may stop. However, in case you continue to skip payments in the new plan, the foreclosed process can pick up exactly where it left off.
Spot on with this write-up, I really believe this website needs a lot more attention. I’ll probably be returning to read through more, thanks for the advice!
Excellent site you’ve got here.. It’s difficult to find excellent writing like yours these days. I seriously appreciate individuals like you! Take care!!
Loving the information on this site, you have done outstanding job on the posts .
Cheers for this material I has been browsing all Msn in order to find it!
Undeniably believe that which you said. Your favorite justification seemed to be on the internet the easiest thing to be aware of. I say to you, I definitely get annoyed while people consider worries that they plainly don’t know about. You managed to hit the nail upon the top and also defined out the whole thing without having side effect , people can take a signal. Will likely be back to get more. Thanks
Hey there! I just want to offer you a huge thumbs up for the excellent info you’ve got here on this post. I am coming back to your web site for more soon.
This post is very helpful! I appreciate the effort you put into making it clear and easy to understand. Thanks for sharing!
You need to take part in a contest for one of the highest quality blogs on the web. I am going to recommend this site!
Great article! I learned a lot from your detailed explanation. Looking forward to more informative content like this!
An outstanding share! I’ve just forwarded this onto a coworker who had been doing a little homework on this. And he actually ordered me dinner simply because I stumbled upon it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanx for spending the time to discuss this topic here on your web site.
I want to express thanks to you just for rescuing me from this particular instance. Just after searching through the online world and coming across tips which were not beneficial, I believed my life was over. Existing without the answers to the problems you’ve solved by means of the article content is a critical case, and the kind which may have in a wrong way affected my entire career if I had not noticed your website. Your actual natural talent and kindness in handling the whole thing was vital. I am not sure what I would have done if I hadn’t come across such a point like this. I can at this time relish my future. Thank you very much for your skilled and effective help. I won’t think twice to endorse your web sites to anybody who will need assistance about this area.
Thanx for a very informative blog. Where else may I get that type of information written in such a perfect approach? I’ve a challenge that I’m just now running on, and I’ve been on the look out for such information.
Hello! I’ve been reading your web site for a while now and finally got the courage to go ahead and give you a shout out from Kingwood Texas! Just wanted to say keep up the good work!
Strong blog. I acquired variant nice info. I?ve been keeping an eye fixed on this technology for a few time. It?utes attention-grabbing the method it retains completely different, yet a few of the primary components remain the same. have you observed lots modification since Search engines created their own latest purchase in the field?
Thanks for all of the labor on this site. My mother take interest in conducting research and it’s simple to grasp why. Many of us hear all regarding the lively mode you deliver great items on the website and as well as attract participation from others on the matter then my princess is in fact becoming educated a lot. Take advantage of the rest of the new year. You have been carrying out a remarkable job.
It??s nice to definitely locate a blog the spot that the blogger is . Appreciation for making your blog site.
Awesome, that is certainly what I was scanning pertaining to! You recently conserved me much rooting all over
Hello! I just would like to give a enormous thumbs up for the excellent information you’ve here on this post. I will likely be coming back to your weblog for much more soon.
i don’t like razors so i always use hair clippers to cut my hair;
Hi there! I could have sworn I’ve visited this website before but after going through many of the posts I realized it’s new to me. Anyways, I’m certainly delighted I stumbled upon it and I’ll be bookmarking it and checking back often!
Hello! I could have sworn I’ve been to this web site before but after going through a few of the posts I realized it’s new to me. Anyways, I’m definitely delighted I came across it and I’ll be bookmarking it and checking back frequently.
Spot on with this write-up, I absolutely believe that this amazing site needs a lot more attention. I’ll probably be returning to read through more, thanks for the advice!
Very interesting points you have observed , thanks for posting .
This web-site is actually a walk-through rather than the info you desired concerning this and didn’t know who to inquire about. Glimpse here, and you’ll absolutely discover it.
Immediately after study a couple of of the blog posts on your internet site now, and I truly like your way of blogging. I bookmarked it to my bookmark site list and will be checking back soon. Pls check out my web website as well and let me know what you think.
Theoharis, Mark. “Legal guidelines on Bankruptcy Fraud.” Criminal Protection Lawyer.
Saved as a favorite, I really like your web site!
On the morning of December 25, Washington ordered his Continental Army troops to prepare three days’ food and issued orders that every soldier be outfitted with recent flints for their muskets.
You made some tight points there. I looked on the web for the issue and found most individuals will approve with your blog.
hey there and thanks to your info – I have definitely picked up anything new from right here. I did then again experience several technical issues the usage of this web site, since I skilled to reload the site lots of instances previous to I may just get it to load correctly. I had been pondering if your web host is OK? Not that I am complaining, but sluggish loading instances occasions will sometimes impact your placement in google and could damage your high-quality score if advertising and with Adwords. Well I’m including this RSS to my email and can glance out for much extra of your respective exciting content. Make sure you update this once more soon..
Hiya, I’m really glad I’ve found this info. Today bloggers publish just about gossips and web and this is really annoying. A good website with exciting content, this is what I need. Thanks for keeping this web-site, I will be visiting it. Do you do newsletters? Can’t find it.
Pretty! This has been a really wonderful post. Thank you for supplying this info.
How much of an unique article, keep on posting better half
I am usually to running a blog and i really admire your content. The write-up has really highs my interest. I will bookmark your own web site and maintain checking for brand spanking new data.
After I initially commented I seem to have clicked the -Notify me when new comments are added- checkbox and from now on each time a comment is added I get four emails with the same comment. There has to be an easy method you are able to remove me from that service? Appreciate it.
I have been surfing online more than three working hours today, however I never found any kind of interesting document like your own. It is quite worth enough to me. Personally, if all web owners and blog writers created great articles as you did, the internet will be a lot more useful than previously.
Good publish, introducing this to my website today, cheers. >
I’ve been visiting your blog for a while now and I always find a gem in your new posts. Thanks for sharing.
I want to to thank you for this fantastic read!! I definitely loved every little bit of it. I have you book-marked to check out new stuff you post…
It’s rare knowledgeable people with this topic, however, you be understood as there’s more you are referring to! Thanks
Great info. Lucky me I came across your website by accident (stumbleupon). I’ve book-marked it for later!
There is definately a lot to find out about this issue. I love all of the points you’ve made.
I like this post, enjoyed this one appreciate it for putting up.
Sweet website , super design , real clean and utilize friendly .
Everything you need to know about News in a great way.
This is the perfect blog for anyone who wishes to find out about this topic. You realize a whole lot its almost tough to argue with you (not that I personally would want to…HaHa). You definitely put a new spin on a topic which has been written about for decades. Excellent stuff, just wonderful.
I could not refrain from commenting. Perfectly written!
Can I just say what a relief to discover an individual who actually understands what they are talking about on the net. You certainly understand how to bring a problem to light and make it important. A lot more people should read this and understand this side of the story. I can’t believe you are not more popular given that you definitely have the gift.
He invented the security catch.
What sort of hair texture do you’ve got?
A blog like yours should be earning much money from adsense.~**;’
very good publish, i definitely love this web site, keep on it
I blog frequently and I genuinely thank you for your content. The article has really peaked my interest. I will bookmark your blog and keep checking for new details about once per week. I subscribed to your Feed too.
A powerful share, I simply given this onto a colleague who was doing a bit of analysis on this. And he actually purchased me breakfast because I found it for him.. smile. So let me reword that: Thnx for the deal with! However yeah Thnkx for spending the time to discuss this, I feel strongly about it and love studying extra on this topic. If potential, as you become experience, would you thoughts updating your weblog with more details? It is extremely helpful for me. Massive thumb up for this blog post!
There’s definately a great deal to learn about this subject. I love all the points you made.
The next time I read a blog, Hopefully it doesn’t disappoint me just as much as this one. I mean, I know it was my choice to read, however I really thought you would have something helpful to say. All I hear is a bunch of complaining about something you could fix if you weren’t too busy seeking attention.
there are many sites on the internet that offers downloadable movies, some are even offering the latest movies*
Everyone loves it whenever people come together and share ideas. Great site, keep it up.
I need to admit that that is one wonderful insight. It surely gives a company the opportunity to have in around the ground floor and really take part in making a thing special and tailored to their needs.
Your style is so unique compared to other folks I’ve read stuff from. I appreciate you for posting when you’ve got the opportunity, Guess I will just book mark this blog.
Everyone loves it whenever people get together and share opinions. Great website, continue the good work!
You ought to be a part of a contest for one of the greatest websites online. I am going to recommend this blog!
Very good blog post. I absolutely appreciate this site. Keep it up!
Good post! We are linking to this great content on our website. Keep up the good writing.
This is a topic that is close to my heart… Many thanks! Exactly where can I find the contact details for questions?
I like reading through a post that can make people think. Also, thank you for permitting me to comment.
Can I simply just say what a relief to uncover somebody who really understands what they are talking about on the web. You actually know how to bring a problem to light and make it important. More and more people should look at this and understand this side of the story. It’s surprising you are not more popular since you surely have the gift.
I really want to thank you for yet another great informative post, I’m a loyal visitor to this blog and I can’t stress enough how much valuable information I’ve learned from reading your content. I really appreciate all the effort you put into this great site.
Great post! We are linking to this great content on our site. Keep up the good writing.
This website definitely has all of the information and facts I wanted concerning this subject and didn’t know who to ask.
Hi, I do think this is a great site. I stumbledupon it 😉 I may return yet again since I bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to help others.
The market capitalization of a cryptocurrency is calculated by multiplying the price by the number of coins in circulation.
Your style is really unique in comparison to other folks I have read stuff from. Thanks for posting when you’ve got the opportunity, Guess I’ll just bookmark this page.
The state’s economic analysis shows a thriving economy with strong sectors in pharmaceuticals, finance and information technology, making it easily one of the richest states in America.
I absolutely love your site.. Great colors & theme. Did you make this amazing site yourself? Please reply back as I’m planning to create my own personal blog and want to learn where you got this from or what the theme is named. Thanks!
Though the Soviets will lose more tanks than the Germans, they’ll substitute them more shortly.
The American Institute of Certified Public Accountants started codifying the Statements on Auditing requirements semiannually in 1976.
This website certainly has all the information I needed concerning this subject and didn’t know who to ask.
I like it when individuals come together and share ideas. Great blog, stick with it!
I needed to thank you for this wonderful read!! I absolutely enjoyed every little bit of it. I have you book-marked to check out new stuff you post…
Hi! I simply wish to give you a huge thumbs up for your great info you’ve got here on this post. I am returning to your site for more soon.
Good post. I learn something new and challenging on sites I stumbleupon on a daily basis. It’s always interesting to read through articles from other writers and practice something from their web sites.
The bread Columbus ate was “hardtack,” an unleavened, laborious, thick bread that might survive a long sea journey without spoiling.
By analyzing these factors, retailers can develop regression models that provide valuable insights into the factors influencing sales, helping them make informed decisions on inventory levels, promotional strategies, and resource allocation.
They will conduct a complete evaluation and provide an accurate prognosis, which is essential for growing an efficient treatment plan.
I truly love your website.. Great colors & theme. Did you create this website yourself? Please reply back as I’m planning to create my own personal blog and want to know where you got this from or exactly what the theme is named. Cheers.
I really like what you guys tend to be up too.
This sort of clever work and coverage! Keep up the excellent works guys I’ve you guys to blogroll.
Pretty! This has been a really wonderful article.
Many thanks for supplying this info.
I agree entirely with this. It’s something I saw discussed in an article on Thew14.com, and I think it’s a very well-argued perspective.
Having read this I believed it was rather enlightening. I appreciate you taking the time and energy to put this short article together. I once again find myself personally spending way too much time both reading and leaving comments. But so what, it was still worthwhile.
I’m pretty pleased to discover this great site. I need to to thank you for your time for this particularly wonderful read!! I definitely really liked every part of it and I have you book marked to see new things on your website.
I blog quite often and I genuinely thank you for your information. Your article has truly peaked my interest. I am going to bookmark your blog and keep checking for new information about once per week. I subscribed to your Feed as well.
Great post. I’m going through some of these issues as well..
I’m amazed, I have to admit. Rarely do I come across a blog that’s equally educative and entertaining, and let me tell you, you’ve hit the nail on the head. The problem is something that too few folks are speaking intelligently about. I’m very happy I came across this during my search for something concerning this.
After I originally commented I seem to have clicked on the -Notify me when new comments are added- checkbox and from now on each time a comment is added I recieve 4 emails with the exact same comment. Perhaps there is an easy method you can remove me from that service? Appreciate it.
Very good article! We will be linking to this particularly great article on our site. Keep up the great writing.
Good write-up. I absolutely appreciate this website. Stick with it!
Franchising now in current times has proved to be profit making and business expansion for every entity.
You have made some decent points there. I checked on the internet for additional information about the issue and found most individuals will go along with your views on this website.
Department of the Treasury Office of Terrorism and Financial Intelligence.
After I initially left a comment I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on every time a comment is added I receive 4 emails with the exact same comment. There has to be a way you can remove me from that service? Cheers.
Thanks very interesting blog!
You made some decent points there. I checked on the web for additional information about the issue and found most people will go along with your views on this web site.
A fascinating discussion is definitely worth comment. I do think that you need to publish more about this subject matter, it might not be a taboo matter but usually people don’t speak about such issues. To the next! Kind regards!
Good day! I could have sworn I’ve been to your blog before but after browsing through many of the articles I realized it’s new to me. Anyways, I’m certainly happy I stumbled upon it and I’ll be bookmarking it and checking back often.
Normally I do not learn article on blogs, however I would like to say that this write-up very compelled me to check out and do it! Your writing style has been amazed me. Thank you, very nice post.
A motivating discussion is worth comment. I think that you ought to write more
on this topic, it may not be a taboo matter but usually people don’t speak about such subjects.
To the next! All the best!!
Right here is the perfect blog for everyone who wishes to find out about this topic. You know a whole lot its almost tough to argue with you (not that I personally will need to…HaHa). You definitely put a new spin on a topic that’s been written about for ages. Great stuff, just wonderful.
On the draw back, they can be pricey to repair if you’ll want to entry an underground portion of the system.
Within the opening recreation, India defeated Cambodia 6-zero with Chhetri scoring two objectives.
Excellent site you have got here.. It’s difficult to find quality writing like yours these days. I really appreciate people like you! Take care!!
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
An impressive share! I have just forwarded this onto a friend who was conducting a little homework on this. And he in fact ordered me dinner because I discovered it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending time to talk about this matter here on your blog.
Having read this I thought it was rather informative. I appreciate you taking the time and effort to put this article together. I once again find myself spending a lot of time both reading and posting comments. But so what, it was still worth it.
This excellent website really has all of the information and facts I needed about this subject and didn’t know who to ask.
The very next time I read a blog, I hope that it doesn’t fail me just as much as this particular one. I mean, I know it was my choice to read through, nonetheless I truly believed you would have something interesting to talk about. All I hear is a bunch of crying about something you could fix if you weren’t too busy looking for attention.
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I’m going to revisit once again since i have bookmarked it. Money and freedom is the greatest way to change, may you be rich and continue to help other people.
Nice post. I learn something new and challenging on blogs I stumbleupon on a daily basis. It will always be interesting to read articles from other writers and use something from other websites.
Excellent post! We are linking to this particularly great content on our site. Keep up the good writing.
Good article. I certainly love this site. Stick with it!
Interesting perspective!
Great article! I learned a lot from your detailed explanation. Looking forward to more informative content like this!
Hi there! I could have sworn I’ve visited this web site before but after going through some of the articles I realized it’s new to me. Regardless, I’m certainly delighted I found it and I’ll be book-marking it and checking back regularly!
sex nhật hiếp dâm trẻ em ấu dâm buôn bán vũ khí ma túy bán súng sextoy chơi đĩ sex bạo lực sex học đường tội phạm tình dục chơi les đĩ đực người mẫu bán dâm
This was a great read! Your insights are truly helpful and make complex topics easy to understand. Looking forward to more!
I appreciate the depth of research in this article. It’s both informative and engaging. Keep up the great work!
Great article! I learned a lot from your detailed explanation. Looking forward to more informative content like this!
Wonderful post! We will be linking to this great article on our website. Keep up the good writing.
Having read this I believed it was rather enlightening. I appreciate you spending some time and energy to put this article together. I once again find myself spending a significant amount of time both reading and leaving comments. But so what, it was still worthwhile.
Good post. I learn something totally new and challenging on sites I stumbleupon every day. It will always be interesting to read through content from other writers and practice something from other web sites.
You ought to be a part of a contest for one of the highest quality websites on the internet. I am going to highly recommend this blog!
I appreciate the depth of research in this article. It’s both informative and engaging. Keep up the great work!
May I simply just say what a comfort to discover someone who truly understands what they’re discussing on the web. You actually realize how to bring an issue to light and make it important. A lot more people must check this out and understand this side of the story. I was surprised you are not more popular since you surely have the gift.
This post is very helpful! I appreciate the effort you put into making it clear and easy to understand. Thanks for sharing!
This is the right website for anyone who wants to find out about this topic. You understand a whole lot its almost hard to argue with you (not that I actually would want to…HaHa). You definitely put a fresh spin on a subject that’s been discussed for many years. Wonderful stuff, just wonderful.
Well-written and insightful! Your points are spot on, and I found the information very useful. Keep up the great work!
Halloween Horror Nights 13 once more occurred at Islands of Journey.
Everything is very open with a really clear explanation of the challenges. It was truly informative. Your website is very helpful. Thank you for sharing.
You’ve made some decent points there. I looked on the internet for additional information about the issue and found most people will go along with your views on this website.
Good post. I learn something new and challenging on blogs I stumbleupon everyday. It’s always interesting to read articles from other writers and practice a little something from their websites.
Excellent post. I absolutely appreciate this website. Stick with it!
Aw, this was a very good post. Finding the time and actual effort to make a very good article… but what can I say… I put things off a whole lot and don’t seem to get nearly anything done.
You need to be a part of a contest for one of the best websites on the internet. I will recommend this blog!
I quite like reading a post that will make men and women think. Also, thanks for allowing for me to comment.
Regular meeting goers will know the significance of constructing the time spent around the boardroom table as productive as attainable.
I’d like to thank you for the efforts you’ve put in writing this website. I really hope to check out the same high-grade content from you in the future as well. In fact, your creative writing abilities has motivated me to get my own blog now 😉
Roy died June 15, 1960.
British forces then reached Damascus, following which the French had been escorted and confined to their barracks.
Your style is unique in comparison to other people I have read stuff from. Thanks for posting when you have the opportunity, Guess I’ll just book mark this page.
Do you know what a sky wheelie is?
He further said that bitcoin is expected to clear $42.6K for a revised upside target of $51K.
There are some benefits or rewards for Umrah/significance of Umrah.
Can you might have 2 resumes on certainly?
To keep a minimalist design from looking too cold and sterile, add a few accents in a couple of different colors.
And irons, of course, use steam to work the wrinkles out of fabrics when dryers do not cut it.
The most well liked temperature ever recorded in Australia happened in the small, distant outback town of Oodnadatta, which is in South Australia.
The album, titled One, is about man’s relationship with God from his Christian perspective and was launched on November 2, 2004.
However finally, the waiters would return if diners flooded the restaurant because of food high quality which might presumably mean more profit and better wages for all.
Aw, this was a really nice post. Taking the time and actual effort to make a top notch article… but what can I say… I hesitate a whole lot and don’t seem to get nearly anything done.
To investors, the bid-ask spread can be a investing cost.
Aw, this was an exceptionally nice post. Taking the time and actual effort to make a top notch article… but what can I say… I put things off a whole lot and don’t manage to get anything done.
Pallbearers are Thomas Jones, Jr., Brandon Minner, William Snyder Jr., Chris Morgan, Nate Silva and Trent Stuart.
The template here comes up with not one however two football grid cards for your NFL soccer video games.
This only means that you must buy with quality in mind first and price as a secondary consideration only.
Scientists continue to discover the area, however neither a meteorite nor a crater have ever been found.
Fantastic post! The information you shared is really valuable and well-explained. Thanks for putting this together!
This post is very helpful! I appreciate the effort you put into making it clear and easy to understand. Thanks for sharing!
This is the perfect site for anybody who would like to understand this topic. You understand a whole lot its almost hard to argue with you (not that I personally would want to…HaHa). You certainly put a fresh spin on a topic which has been written about for ages. Great stuff, just great.
After I initially commented I seem to have clicked the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I recieve 4 emails with the exact same comment. There has to be a way you can remove me from that service? Thanks.
Until the present economic downturn it was not particularly difficult to arrange a very large mortgage in comparison to your income.
Richard Allen later grew to become a preacher in the Methodist Church in Philadelphia, co-founder of the Free African Society, and the founder and first bishop of the African Methodist Episcopal Church, the primary African American denomination in the United States.
Once upon a time it was the pocket watch; then a steam engine; later still a phone alternate; and now we should take care of computer systems.
However I do assume there are human prices to conflating thought of pragmatism with a scarcity of cautious, step-by-step thought.
Everything is very open with a really clear explanation of the challenges. It was truly informative. Your website is very helpful. Many thanks for sharing.
Full assembly is the buyer’s responsibility, and they can either keep the stock Mazda engine, or substitute a variety of more powerful options.
I could not resist commenting. Well written!
Commerce Department, consumer spending stagnated in May.
Saved as a favorite, I like your website.
Lebanon County Correctional Facility Women’s Chaplain.
The DJIA and Nasdaq Composite, both reached an all-time high on 12 July and 8 August respectively.
German Fallschirmjäger from the 7th Flieger and 22nd Air Touchdown divisions underneath Kurt Scholar executed surprise landings on the Hague, on the road to Rotterdam, and towards the Belgian Fort Eben-Emael to facilitate Military Group B’s advance.
One of the best part of it’s when your ready to buy online you might be given the chance to get cash back from each transaction you make.
Aw, this was an extremely good post. Taking the time and actual effort to generate a really good article… but what can I say… I put things off a whole lot and never manage to get nearly anything done.
Hi, I do think this is an excellent web site. I stumbledupon it 😉 I’m going to return once again since i have book marked it. Money and freedom is the greatest way to change, may you be rich and continue to guide others.
Climate change is projected to increase the variability of rain.
Tuesday in Bettes Chapel with Bro.
Funeral services will probably be held Saturday, Aug 9, eleven a.m.
Following the trade wars and adjusts of punches tossed by the US and China, the assembling area may endure a shot via the gadgets division.
I wanted to thank you for this very good read!! I definitely loved every bit of it. I’ve got you saved as a favorite to look at new things you post…
Requested if he really thought, deep down, Ronnie beloved him as much as his biological children, Jamie says: ‘I knew I wasn’t his blood.
Way cool! Some very valid points! I appreciate you penning this article plus the rest of the website is extremely good.
This is a topic which is close to my heart… Many thanks! Where are your contact details though?
Great web site you have here.. It’s difficult to find high-quality writing like yours nowadays. I truly appreciate people like you! Take care!!
I must thank you for the efforts you have put in writing this website. I really hope to check out the same high-grade blog posts from you later on as well. In truth, your creative writing abilities has motivated me to get my own website now 😉
For some actual shorthand, name it “James Bond meets The X-Recordsdata.” (Remember that seemingly innocent claim that Deus Ex is set in the true world.
Excellent article! We are linking to this particularly great post on our site. Keep up the great writing.
Nihilus imbued his darkish soul into his mask and robes and had the facility to drain the life power out of any dwelling thing.
With just seven of their 20 factors received on residence soil earlier than kick-off, the Shots have been desperate to appease the increasingly restless supporters, especially within the wake of back-to-back 3-0 defeats by Macclesfield and Forest Green.
Prices also vary primarily based on whether the client additionally has Verizon phone service.
It focuses primarily on when and how an organization can best hedge against exposure to fuel price volatility.
Pretty! This was an extremely wonderful post. Thank you for supplying this information.
Florence Elizabeth Breakie, JP.
I could not refrain from commenting. Perfectly written!
Pretty! This has been an incredibly wonderful article. Many thanks for supplying this info.
The next-generation technology, LED bulbs, can last a purported 25,000 hours.
That is a great tip especially to those new to the blogosphere. Short but very accurate info… Appreciate your sharing this one. A must read article.
Starting in the 2018 racing season, the template used by Chevrolet drivers in the NASCAR top-tier circuit – the Monster Energy Cup Series – was changed from the Chevy SS to the Camaro ZL1.
When I originally left a comment I seem to have clicked on the -Notify me when new comments are added- checkbox and from now on each time a comment is added I get 4 emails with the same comment. Perhaps there is an easy method you are able to remove me from that service? Thank you.
We use the love of God and our love as a weapon in opposition to the forces of evil.
This give also enable them bingle out those people who offering the selfsame recommendation to all their clients since all not like investors quantity with diametric needs.
On May 29, 2022, Horvath came on instead in Forest’s 1-zero play-off remaining victory over Huddersfield City at Wembley Stadium in the 90th minute, as a consequence of an harm for starting goalkeeper Brice Samba.
According to the Coast Guard’s webpage, “Compared to legacy cutters, the NSCs’ design offers higher sea-retaining and better sustained transit speeds, larger endurance and range, and the ability to launch and get well small boats from astern, in addition to aviation help services and a flight deck for helicopters and unmanned aerial vehicles.” Their designation is WMSL (Maritime Safety, Giant).
This will fall if interest charges fall, however it is still going to be lots better than any investment you might make.
I find it tough to imagine a world in which Mastodon posts federated into Threads don’t present content material against which Meta can run advertisements-and, less simplistically, a world wherein Threads’ users’ interactions with Mastodon posts don’t provide behavioral indicators that enable Meta to supply their purchasers more fantastic-grained concentrating on data.
Knowing how to negotiate will help you save a lot of money and get extra benefits such as parking spaces, furniture, and other perks.
Now, go and grab your own trading association and be accelerating on this craft.
Whether you need to work for an NGO that promotes women’s empowerment tasks in other international locations, construct expertise in a business business, or work for a chopping-edge begin-up, there are numerous options accessible.
Further, real estate agents can assist you with quick and easy financing so that you can realize all your dreams of owning your dream home.
Consolidate all of the invoices – You will need to make sure that your accountants consolidate all the invoices and process them concurrently.
The very next time I read a blog, I hope that it does not disappoint me as much as this one. I mean, Yes, it was my choice to read through, nonetheless I truly believed you would have something helpful to talk about. All I hear is a bunch of moaning about something that you could possibly fix if you were not too busy seeking attention.
VPN-enabled Firewall – This is a traditional firewall defending visitors between networks, but with the added characteristic of managing traffic utilizing protocols specific to VPNs.
Excellent article. I absolutely appreciate this site. Thanks!
The very next time I read a blog, I hope that it doesn’t disappoint me as much as this particular one. I mean, Yes, it was my choice to read, nonetheless I truly thought you would probably have something helpful to talk about. All I hear is a bunch of complaining about something you could possibly fix if you were not too busy looking for attention.
You made some good points there. I looked on the internet to find out more about the issue and found most people will go along with your views on this web site.
4. Proto-missions redux. Recreation Developer’s Postmortems sometimes focus in on issues the crew clearly did proper and things the group clearly did wrong.
For individuals with those concerns, Threads federation is a pretty large step towards being in a position to maintain an account on Mastodon (or another fediverse service) and nonetheless find the individuals they wish to interact with-assuming a few of those individuals are on Threads and not solely on Bluesky, Twitter/X, Instagram, and all the opposite non-ActivityPub-powered systems.
Moreover, the workers in these restaurants typically exude genuine warmth and hospitality.
Pretty! This has been an extremely wonderful post. Thanks for supplying this info.
Rowland Milwyn Morris, Sub-Postmaster, Painscastle Sub-Put up Office, Builth Wells, Breconshire.
Aw, this was a really good post. Taking a few minutes and actual effort to create a really good article… but what can I say… I hesitate a whole lot and don’t manage to get anything done.
Very good information. Lucky me I ran across your website by accident (stumbleupon). I have bookmarked it for later!
Reasonably priced Engagement Rings – Uncover a gorgeous assortment of gemstone engagement rings, together with moissanite, opal, and princess minimize designs.
Fired which broke out in each trucks immediately after the head-on crash cremated the bodies of both drivers.
I like it whenever people get together and share ideas. Great blog, stick with it.
Hi, I believe your website could possibly be having web browser compatibility problems. Whenever I take a look at your web site in Safari, it looks fine however, when opening in IE, it has some overlapping issues. I just wanted to give you a quick heads up! Besides that, wonderful site.
Spot on with this write-up, I really believe this amazing site needs far more attention. I’ll probably be returning to read more, thanks for the information!
This step is still where you have to start (meaning it’s no different from if you’d planned to buy or lease a car from a dealership).
Right here is the right website for everyone who wants to find out about this topic. You realize a whole lot its almost hard to argue with you (not that I actually will need to…HaHa). You definitely put a brand new spin on a topic which has been discussed for ages. Great stuff, just great.
You ought to be a part of a contest for one of the finest blogs on the internet. I’m going to highly recommend this web site!
You’re so cool! I do not suppose I have read anything like this before. So nice to discover someone with a few original thoughts on this subject matter. Really.. thanks for starting this up. This web site is one thing that’s needed on the internet, someone with a little originality.
Hey there! I just would like to offer you a huge thumbs up for the great info you have right here on this post. I am returning to your website for more soon.
You need to take part in a contest for one of the finest sites on the web. I most certainly will recommend this website!
Good post. I learn something totally new and challenging on blogs I stumbleupon everyday. It will always be exciting to read content from other writers and practice something from their websites.
Attach an F-channel to the underside outer edge of the fascia board.
An impressive share! I’ve just forwarded this onto a co-worker who was conducting a little research on this. And he in fact ordered me breakfast due to the fact that I discovered it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending some time to discuss this matter here on your blog.
Very nice article. I absolutely love this site. Stick with it!
This is a good tip particularly to those fresh to the blogosphere. Brief but very accurate info… Thanks for sharing this one. A must read post!
After checking out a few of the articles on your web site, I truly like your technique of blogging. I saved it to my bookmark webpage list and will be checking back soon. Please visit my website too and let me know your opinion.
I absolutely love your site.. Very nice colors & theme. Did you develop this website yourself? Please reply back as I’m attempting to create my very own site and would love to find out where you got this from or what the theme is called. Thank you!
Greetings! Very useful advice in this particular article! It’s the little changes that will make the greatest changes. Thanks for sharing!
I used to be able to find good information from your articles.
Spot on with this write-up, I really believe that this amazing site needs a lot more attention. I’ll probably be back again to read more, thanks for the advice.
Europe Incoming, as a leading supplier of pupil Europe tour operates, understands the precise wants and finances constraints of younger travelers.
I blog often and I truly thank you for your information. Your article has truly peaked my interest. I’m going to bookmark your blog and keep checking for new information about once per week. I subscribed to your Feed as well.
After looking into a number of the articles on your blog, I truly like your technique of blogging. I saved as a favorite it to my bookmark site list and will be checking back soon. Take a look at my web site as well and tell me what you think.
I wanted to thank you for this wonderful read!! I certainly loved every little bit of it. I have you book marked to look at new things you post…
I was able to find good advice from your articles.
A motivating discussion is definitely worth comment. There’s no doubt that that you need to write more on this issue, it might not be a taboo matter but generally people don’t discuss such topics. To the next! All the best.
Way cool! Some extremely valid points! I appreciate you writing this article and the rest of the website is extremely good.
Excellent site you have here.. It’s hard to find high quality writing like yours nowadays. I really appreciate people like you! Take care!!
I need to to thank you for this fantastic read!! I absolutely loved every little bit of it. I have got you bookmarked to check out new stuff you post…
I blog frequently and I really thank you for your content. The article has truly peaked my interest. I will take a note of your blog and keep checking for new details about once a week. I subscribed to your Feed as well.
Pretty! This has been an extremely wonderful article. Thank you for supplying this info.
The story and the film are thought-about battle classics and garnered a number of Academy Award nominations, together with one for Best Writing.
An impressive share! I have just forwarded this onto a friend who has been conducting a little research on this. And he actually ordered me dinner because I stumbled upon it for him… lol. So allow me to reword this…. Thanks for the meal!! But yeah, thanx for spending the time to discuss this topic here on your internet site.
Three $10 door prizes!
The agency could be for the want to provide capital, and advantageous information that you just just have presently acquired from other regions.
Excellent web site you’ve got here.. It’s hard to find quality writing like yours these days. I truly appreciate people like you! Take care!!
Hi, I do think this is an excellent site. I stumbledupon it 😉 I’m going to come back once again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to guide others.
Aw, this was an extremely nice post. Finding the time and actual effort to create a really good article… but what can I say… I procrastinate a whole lot and don’t manage to get anything done.
Hey there! I just want to offer you a huge thumbs up for your excellent information you’ve got right here on this post. I am coming back to your web site for more soon.
I used to be able to find good info from your blog articles.
I couldn’t resist commenting. Well written.
AMC brought out the compact Hornet to compete with imports from Japan and Europe in 1970.
Great information. Lucky me I came across your site by chance (stumbleupon). I’ve saved it for later.
Having read this I believed it was extremely informative. I appreciate you spending some time and effort to put this information together. I once again find myself spending way too much time both reading and leaving comments. But so what, it was still worth it!
A motivating discussion is definitely worth comment. I think that you ought to publish more about this issue, it may not be a taboo subject but generally people do not speak about such topics. To the next! Kind regards!
Hello, Neat post. There is an issue along with your site in web explorer, could test this¡K IE still is the marketplace leader and a huge portion of other people will miss your magnificent writing because of this problem.
When I originally commented I clicked the -Notify me when new comments are added- checkbox and after this each time a comment is added I recieve four emails with the exact same comment. Possibly there is that is you are able to get rid of me from that service? Thanks!
Nice post. I learn something new and challenging on sites I stumbleupon on a daily basis. It will always be helpful to read content from other authors and use a little something from their websites.
Burial was within the McHorse cemetery below the course of Wilkerson Funeral Dwelling.
I need to to thank you for this excellent read!! I definitely enjoyed every bit of it. I have got you book-marked to look at new stuff you post…
Hiya! awesome blog! I happen to be a daily visitor to your site (somewhat more like addict ) of this website. Just wanted to say I appreciate your blogs and am looking forward for more to come!
Thanks for your kind data.. I realy appreciate it.. keep it up.
bookmarked!!, I love your web site.
Oh my goodness! Awesome article dude! Thanks, However I am encountering problems with your RSS. I don’t know the reason why I can’t join it. Is there anybody getting similar RSS problems? Anyone that knows the solution can you kindly respond? Thanks!
All the prices of Medicare are usually not fully covered by what you set in over your lifetime.
Its like you read my mind! You appear to know a lot about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a bit, but other than that, this is fantastic blog. A great read. I’ll certainly be back.
When I originally commented I clicked the -Notify me when new surveys are added- checkbox and after this if a comment is added I purchase four emails with the exact same comment. Can there be that is you can remove me from that service? Thanks!
I’m impressed, I must say. Seldom do I come across a blog that’s both equally educative and amusing, and without a doubt, you have hit the nail on the head. The problem is something which not enough people are speaking intelligently about. I’m very happy I stumbled across this during my hunt for something regarding this.
Great post! We are linking to this particularly great article on our website. Keep up the great writing.
maintaining a healthy weight can be tricky because it revolves around genetics and some other factors;;
dining room furnitures should be coated with shellac or varnish in order to preserve the wood grains::
Aw, this was an extremely good post. Spending some time and actual effort to produce a really good article… but what can I say… I hesitate a whole lot and don’t seem to get anything done.
Your style is so unique in comparison to other people I’ve read stuff from. Thanks for posting when you have the opportunity, Guess I will just book mark this web site.
An impressive share! I have just forwarded this onto a coworker who has been conducting a little homework on this. And he actually bought me dinner due to the fact that I stumbled upon it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanks for spending some time to talk about this matter here on your site.
I have to thank you for the efforts you have put in penning this website. I’m hoping to view the same high-grade blog posts from you later on as well. In fact, your creative writing abilities has inspired me to get my very own site now 😉
There’s definately a lot to learn about this topic. I love all of the points you have made.
Right here is the perfect site for anybody who wishes to understand this topic. You understand so much its almost tough to argue with you (not that I personally will need to…HaHa). You definitely put a fresh spin on a topic that has been written about for years. Wonderful stuff, just great.
An intriguing discussion is definitely worth comment. There’s no doubt that that you need to publish more on this subject, it may not be a taboo subject but generally folks don’t discuss such subjects. To the next! Cheers.
It’s difficult to find experienced people on this topic, however, you sound like you know what you’re talking about! Thanks
The organization later confirmed that Stalions was the main focus of the investigation, and was accused of stealing opposing groups’ alerts at their video games, some of which he attend incognito.
Your style is unique in comparison to other people I have read stuff from. Thank you for posting when you have the opportunity, Guess I will just bookmark this site.
Greetings! Very useful advice in this particular post! It is the little changes that produce the most important changes. Thanks for sharing!
An outstanding share! I have just forwarded this onto a colleague who has been doing a little homework on this. And he actually bought me dinner simply because I found it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanks for spending some time to discuss this issue here on your internet site.
Howdy! This post couldn’t be written much better! Reading through this article reminds me of my previous roommate! He constantly kept preaching about this. I most certainly will forward this information to him. Pretty sure he will have a very good read. Thanks for sharing!
After looking into a number of the blog posts on your website, I seriously like your way of blogging. I saved it to my bookmark webpage list and will be checking back in the near future. Take a look at my website too and tell me how you feel.
This is a topic that is close to my heart… Best wishes! Exactly where are your contact details though?
After looking at a few of the blog posts on your site, I honestly like your way of writing a blog. I saved as a favorite it to my bookmark website list and will be checking back in the near future. Please check out my website as well and let me know how you feel.
An interesting discussion is worth comment. I believe that you should publish more about this subject matter, it might not be a taboo subject but usually people do not speak about these issues. To the next! Kind regards.
This site really has all of the info I wanted about this subject and didn’t know who to ask.
I really like reading an article that will make men and women think. Also, thanks for allowing me to comment.
I like looking through an article that can make men and women think. Also, many thanks for permitting me to comment.
Some really wondrous work on behalf of the owner of this site, perfectly great subject material .
Whole Management Group is a full service Occasion and Travel company.
By means of the influence of A.W.Pugin, John Ruskin, and the Oxford Motion, it was thought-about through the mid-19th century that the one applicable type in which a church must be constructed was Gothic.
Serving shoppers all through Florida and across the nation.
Does your blog have a contact page? I’m having a tough time locating it but, I’d like to send you an e-mail. I’ve got some suggestions for your blog you might be interested in hearing. Either way, great website and I look forward to seeing it expand over time.
I would like to show my thanks to you just for bailing me out of this problem. Right after researching through the world wide web and seeing strategies which are not helpful, I figured my entire life was gone. Existing minus the approaches to the issues you’ve fixed through your main guideline is a crucial case, and ones that would have in a negative way damaged my entire career if I hadn’t discovered your website. Your primary ability and kindness in playing with all things was precious. I am not sure what I would have done if I hadn’t come across such a solution like this. I’m able to at this moment look forward to my future. Thanks for your time very much for this impressive and result oriented guide. I won’t be reluctant to refer the sites to any person who should receive direction on this problem.
First, new individuals joined the crew, with new ideas.
For anybody who is considering about external complications, sometimes be tough amaze those to realize to produce just a single weed in this very flowing usually requires eleven liters concerning gasoline to. dc free mommy blog giveaways family trip home gardening house power wash baby laundry detergent
The ideas you provided here’s extremely precious. It turned out a real pleasurable surprise to get that awaiting me while i woke up today. They may be constantly to the level and easy to be aware of. Thanks plenty for your valuable ideas you’ve got shared in this article.
Please let me know if you’re looking for a article author for your weblog. You have some really good posts and I believe I would be a good asset. If you ever want to take some of the load off, I’d love to write some articles for your blog in exchange for a link back to mine. Please send me an email if interested. Thanks!
From all the blogs I’ve read lately, this at one seems to be the most moving – it gave me something to consider about. [Reply]
I am unable to read articles online very often, but I’m glad I did today. This is very well written and your points are well-expressed. Please, don’t ever stop writing.
I must show some appreciation to the writer for bailing me out of such a problem. After exploring through the internet and getting principles that were not productive, I assumed my life was gone. Being alive devoid of the answers to the difficulties you’ve resolved by way of this report is a crucial case, and the kind that might have in a negative way affected my career if I had not noticed your blog post. Your primary training and kindness in maneuvering all things was very useful. I don’t know what I would have done if I had not come across such a stuff like this. I can at this moment look forward to my future. Thank you so much for the expert and results-oriented help. I will not hesitate to suggest your web page to any individual who needs to have guidelines on this topic.
I am typically to blogging i genuinely appreciate your posts. This content has really peaks my interest. My goal is to bookmark your website and keep checking achievable info.
Excellent read, I merely passed this onto a colleague who was doing little research on that. And the man actually bought me lunch because I found it for him smile So let me rephrase that: Thank you for lunch!
Nice post. I learn something more challenging on different blogs everyday. It would all the time be stimulating to read content from different writers and observe a little something from their store. I’d want to use some with the content material on my blog whether or not you don’t mind. Natually I’ll provide you with a hyperlink on your net blog. Thanks for sharing.
This blog was… how do I say it? Relevant!! Finally I’ve found something which helped me. Many thanks!
I am glad for commenting to let you understand what a notable experience our daughter encountered visiting your webblog. She realized too many things, with the inclusion of what it’s like to possess an excellent giving mood to let other people very easily thoroughly grasp selected complicated subject areas. You actually exceeded her expected results. Thank you for offering those essential, dependable, explanatory and even easy guidance on this topic to Sandra.
Perfect! You assisted give me well read material and a solid understanding of this subject.
bedroom furnitures should be sized up and paired with the color and type of your beddings,
Hello there, have you possibly considered to publish about Nintendo or PS handheld?
How come at this time there zero much more a lot of these websites? Your content are perfect and get to themes or templates, that are unable to always be recognized all over the place. Please continue penning this sort of fantastic materials, it could be absolutely important. The net can be full of incredible waste, seeing that A single will be delighted when you learn anything. Exactly why typically are not there a lot more? Commonly do not abandon me dangling!
Yo!. Certainly liked reading your post. It was very informative and helpful. I hope you do not mind me blogging concerning this post on my personal blog. Will definitely link back to you. Nice site theme! Salamat.
living rooms should be decorated with style that is why i always get some living room decoration idea on the internet`
As soon as I detected this website I went on reddit to share some of the love with them.
Enter the quantities you paid for biomass stoves and biomass boilers that have a thermal efficiency score of at the least 75 (measured by the higher heating worth of the fuel).
Even nevertheless there are lots of decision methods with the purpose of lookup used for non published numbers, but you would approximating rapid stately results to you possibly will look forward to in, you possibly will necessitate with the purpose of desire particular sort of swap telephone search company.
Hello! I merely would want to provide a enormous thumbs up for the great info you have here for this post. I will be coming back to your site to get more soon.
Hey, what kind of anti-spam plugin do you use for your blog.;”:”‘
Needed to post you that bit of note to be able to give thanks over again about the awesome concepts you’ve documented in this case. This is so surprisingly open-handed with you to offer without restraint all that a few people would have marketed as an e-book to earn some cash for themselves, especially considering the fact that you might well have done it in case you considered necessary. The smart ideas likewise served like the easy way to realize that other individuals have the identical desire the same as my own to realize a great deal more on the subject of this problem. I’m sure there are thousands of more enjoyable times up front for folks who take a look at your site.
I actually appreciated studying your website, I discovered it in Yahoo. I recently came acrossa reallyinteresting pdf finder type website, its a pdf lookup engine and I think it is actually incredibly interesting for individuals who like reading through pdfs
I’ve been browsing on-line greater than three hours these days, but I by no means discovered any attention-grabbing article like yours. It is pretty value sufficient for me. Personally, if all webmasters and bloggers made good content as you probably did, the web shall be a lot more useful than ever before.
Nice post. I discover something tougher on diverse blogs everyday. Most commonly it is stimulating to learn content from other writers and use a little something from their website. I’d would rather apply certain using the content in this little blog regardless of whether you do not mind. Natually I’ll offer you a link in your web weblog. Many thanks for sharing.
Saved as a favorite, I really like your website!
Where did you get your information from? A ot of it is true but I would like to check on a couple of things.
Music began playing as soon as I opened up this webpage, so frustrating!
Thanks a bunch for sharing this with all people you actually understand what you’re speaking approximately! Bookmarked. Please additionally consult with my site =). We will have a link exchange arrangement between us!
Wonderful beat ! I would like to apprentice whilst you amend your web site, how can i subscribe for a blog website? The account helped me a applicable deal. I had been tiny bit acquainted of this your broadcast provided shiny transparent idea.
well, earning money is a bit tricky and hard sometimes. you really got to be very creative if you want to earn more::
Good blog you have here.. It’s difficult to find excellent writing like yours nowadays. I truly appreciate individuals like you! Take care!!
Can I just say that of a relief to seek out someone who in fact knows what theyre preaching about on-line. You actually have learned to bring a problem to light making it critical. The best way to must check out this and appreciate this side from the story. I cant think youre not more well-known since you also certainly develop the gift.
usually, the best sounding ringtones are coming from paid ringtone donwload sites,.
There are incredibly a lot of details like this to take into consideration. Which is a great point to raise up. I provide thoughts above as general inspiration but clearly you can find questions such as one you start up the place that the most crucial thing is going to be getting work done in honest very good faith. I don?t determine if guidelines have emerged around stuff like that, but I am certain that the job is clearly identified as a fair game. Both boys and girls have the impact of only a moment’s pleasure, through-out their lives.
Write more, thats all I have to say. Literally, it seems as though you relied on the video to make your point. You definitely know what youre talking about, why waste your intelligence on just posting videos to your blog when you could be giving us something enlightening to read?
Can I simply say what a relief to search out someone who actually is aware of what theyre talking about on the internet. You definitely know methods to bring a difficulty to gentle and make it important. More people have to learn this and understand this facet of the story. I cant imagine youre no more widespread since you definitely have the gift.
I think other web-site proprietors should take this website as an model, very clean and excellent user friendly style and design, as well as the content. You’re an expert in this topic!
I’d also like to say that most of those that find themselves with out health insurance can be students, self-employed and people who are jobless. More than half from the uninsured are really under the age of Thirty-five. They do not come to feel they are needing health insurance since they are young in addition to healthy. Their particular income is typically spent on houses, food, and entertainment. Most people that do go to work either full or not professional are not made available insurance by their jobs so they move without with the rising cost of health insurance in the usa. Thanks for the tips you write about through this website.
i prefer wall clocks with hanging pendulums because they look nice at home**
After looking into a handful of the blog posts on your web page, I honestly appreciate your technique of writing a blog. I bookmarked it to my bookmark webpage list and will be checking back soon. Please check out my website as well and let me know what you think.
What?s Taking place i am new to this, I stumbled upon this I have discovered It absolutely useful and it has aided me out loads. I’m hoping to contribute & help other customers like its aided me. Good job.
Thank you for sharing this good write-up. Very inspiring! (as always, btw)
There is certainly a lot to learn about this issue. I like all the points you made.
When Apple didn’t make computers as well as Local cafe did not help make coffee, how arrive acquired they will become thus prospering? The journey to offer the state-of-the-art and most interesting goods, even though intoxicating, is often a fairly packed location. If possible, Apple and Starbucks built their own niche.
However, since this gives the primary move advantage to Black right away, this isn’t recommended.
An inlaid Japanese jewellery field was the inspiration for this room, filled with a wealth of model and amenities.
Chattanooga has a variety of performing arts in different venues.
And, in fact, it had to work with out breaking the rules of baseball.
In addition they wear stable gold bangles named patlya as well as carved kadas which are called tode.
I was able to find good info from your content.
The primary ship in the fleet to receive all Funship 2.Zero amenities.
Great article! We are linking to this particularly great article on our site. Keep up the good writing.
Good site you have got here.. It’s hard to find high-quality writing like yours nowadays. I honestly appreciate individuals like you! Take care!!
After I initially commented I appear to have clicked on the -Notify me when new comments are added- checkbox and from now on whenever a comment is added I receive four emails with the exact same comment. There has to be a way you can remove me from that service? Cheers.
Very good post! We are linking to this great article on our website. Keep up the good writing.
sugar defender reviews Discovering Sugar
Defender has actually been a game-changer for me, as I
have actually always been vigilant about handling my blood sugar level levels.
I currently really feel empowered and confident in my capacity
to preserve healthy and balanced degrees, and my most current medical examination have actually shown this progression. Having a credible supplement to match my a significant
source of convenience, and I’m really grateful for the substantial distinction Sugar Protector
has actually made in my total wellness.
sugar defender ingredients Finding Sugar Protector has
been a game-changer for me, as I have actually always been vigilant concerning handling my
blood sugar levels. I currently really feel encouraged
and positive in my capability to preserve healthy levels, and my most recent
health checks have mirrored this progression. Having a
trustworthy supplement to complement my a big resource of comfort, and I’m really grateful for
the substantial difference Sugar Defender has made in my total wellness.
Aquarius people worth intellectual connection and seek partners who can engage in deep conversations and share their passion for social justice.
Hi! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my
blog to rank for some targeted keywords but I’m not
seeing very good gains. If you know of any please share.
Thank you! You can read similar art here: Blankets